Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Alicia Hereford, MS4
Peer reviewers: Blake Briggs, MD; Travis Smith, DO
Introduction
Lithium has been around since 1817 and has been the gold standard for the treatment of bipolar disorder since the 1970s as well as other conditions like acute mania and unipolar depression.4,7 Lithium is currently one of the treatment options for acute mania, hypomania, bipolar and unipolar depression, and maintenance therapy for bipolar disorder. Given its narrow therapeutic index, its numerous side effects are well described, and overdose vignettes are classically tested on boards. Toxicities can occur from an acute ingestion or acute on chronic ingestion. Any EM physician worth his salt must be ready to treat it. Why? Because in 2018 alone, there were just over 7000 cases of lithium intoxication in the US alone.
Pharmacokinetics
The exact mechanism of action of lithium is unknown- you will never be tested on it.
What we do know is the gastrointestinal tract rapidly absorbs lithium.2,5 It is neither metabolized nor protein bound, making its bioavailability close to 100%. Lithium has a very narrow therapeutic index, so it comes as no surprise that many patients experience at least one episode of toxicity during chronic lithium therapy.5 Since lithium is not protein or tissue bound, it is distributed throughout the body.2,5 Therapeutic serum levels range between 0.8 to 1.2 mEq/L for most people and levels should not exceed 1.2 mEq/L.2,3,12
It gets rapidly absorbed in the GI tract and excretion is mainly through the kidneys (handled similarly to sodium). Thus, a patient’s renal function determines the elimination half-life which is normally around 24 hours but can increase with age as renal function declines. Chronic toxicity can also increase its half-life to 48 hours or so.2,12 Lithium levels are also affected by salt and water balance. This occurs because of the shared similarities between Li and Na. What factors can lead to increased Li absorption? Anything that can cause sodium and volume depletion. Conditions like vomiting, diarrhea, febrile illness, renal insufficiency, excessive exercise, water restriction, excessive sweating, low sodium diet, and congestive heart failure may enhance lithium reabsorption in the kidneys.2
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Clinical presentation and diagnosis
Lithium poisoning often occurs in vulnerable populations, like those with mental illness and poor living conditions. It can cause a battery of adverse effects that aren’t necessarily associated with toxicity.
Clinical pearl: lithium levels do not always correlate with clinical symptoms. Serum lithium levels reflect only the extracellular lithium concentration, but it’s the intracellular concentration where Li exerts its effect.
Diagnosis of lithium toxicity is clinical and confirmed with serum lithium levels. Toxicity can lead to multisystem dysfunction that is potentially fatal.
Lithium levels do not always correlate with clinical symptoms.5,11 Serum lithium concentrations should be obtained upon presentation and repeated every 2-4 hours.
Lithium levels of 1.5 mEq/L can cause mild toxicity. Levels >2.5 mEq/L are a medical emergency.2
The clinical signs and symptoms of toxicity can vary depending on the type of poisoning: chronic (accidental, due to decreased excretion), acute (often attempted suicide), or acute on chronic (on chronic therapy but ingests a supratherapeutic amount). The table below summarizes the difference in these three types of lithium toxicities.
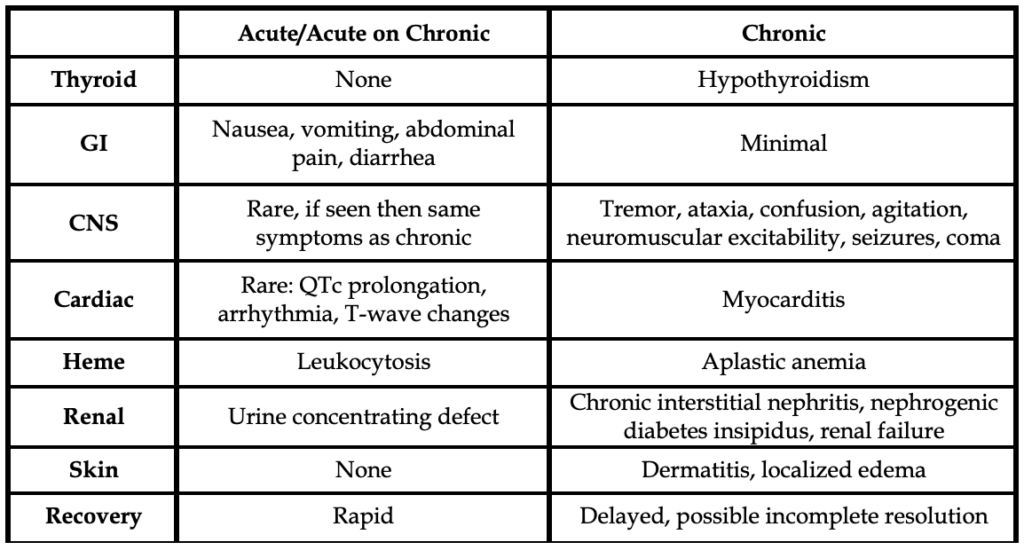
Chronic lithium poisoning is the most common cause of toxicity.4 For this etiology, lithium serum levels correlate more closely to clinical signs seen.4,5 In chronic lithium toxicity, neurologic signs and symptoms (i.e., tremor, sluggishness, ataxia, confusion, agitation, and/or neuromuscular excitability) are usually evident on presentation as they have had time to develop symptoms gradually.
Severe cases of lithium toxicity can result in seizures, nonconvulsive status epilepticus, encephalopathy, and coma.5,6 With treatment, resolution of neurological may take weeks. Sometimes it might not fully resolve.
Polyuria and polydipsia can be seen in patients on chronic lithium therapy. These patients are at risk for development of nephrogenic or central diabetes insipidus.8Chronic therapy can also lead to thyroid dysfunction, usually hypothyroidism.9,10 These conditions can be both a result of chronic lithium therapy and the cause of lithium toxicity.
Acute lithium toxicity
Patient history and recent illnesses are important to ask about. The clinical presentation is normally gastrointestinal signs and symptoms such as nausea, vomiting, abdominal pain, and diarrhea.6 These types of toxicity are usually due to an acute overdose or decline in renal function.5 Vomiting and diarrhea can cause a vicious cycle of worsening dehydration and compromised renal function, impairing the ability to excrete lithium.
Neurologic changes are also rarely seen on initial presentation as these take time to develop. The neurologic signs and symptoms are the same as those described above.
Arrhythmia, prolonged QTc interval, bradycardia, and other EKG changes are possible, but rarely seen in acute toxicity.5
You can usually confirm toxicity based on the lithium serum concentration.5 Of note, a single normal lithium concentration does not rule out lithium toxicity.
Management
As always, the ABCs are our friend and should be used for any poisoned patient: assess and stabilize.2,4,5 Any drug that impairs kidney function should be ceased.
Of course, you will order the usual battery of toxicology panels and EKG to rule out co-ingestion.
Since toxicity can occur with therapeutic lithium levels, treatment should not only be based on lithium concentration, but also clinical signs and symptoms.
Intravenous fluids are initiated at twice the maintenance rate for roughly 2-3 liters to replace gastrointestinal losses from vomiting and diarrhea; this also helps to maintain the glomerular filtration rate (GFR).5 IV crystalloid hydration is essential to enhance lithium clearance. In patients suffering from nephrogenic diabetes insipidus, serum sodium must be watched closely.
Remember that activated charcoal does not help.
In those who present with ingestion of large, extended-release preparations (10-15 tablets), whole bowel irrigation (WBI) with polyethylene glycol solution (PEG) can be used in awake, asymptomatic patients presenting within 3 hours of ingestion.4 This really gets into the weeds of lithium management, and this is quite a select group of patients. More commonly patients present to the ED >3 hours after ingestion with symptoms.
It is important to consult nephrology early, as patients might need hemodialysis. Hemodialysis is performed for the following:
-serum lithium levels above 4.5 mEq/L no matter patient clinical status
-for serum lithium concentrations above 2.5 mEq/L with clinical signs of lithium toxicity
-any renal insufficiency (Cr>2 mg/dL)
-any conditions limiting lithium excretion, or other conditions limiting aggressive IV fluid hydration (e.g., heart failure).5
Disposition
It’s recommended that any patient with an intentional ingestion have a psychiatric evaluation. Irrespective of lithium concentration if patients are symptomatic due to lithium toxicity they are admitted. Patients are admitted to the ICU if they have severe symptoms such as altered mental status or seizures.5 Once patients are asymptomatic and have a lithium level < 1.5 mEq/L, discharge may be appropriate.5
References
1 Kelleher SP, Raciti A, Arbeit LA. Reduced or absent serum anion gap as a marker of severe lithium carbonate intoxication. Arch Intern Med. 1986;146(9):1839-1840.
2 Bipolar disorder in adults and lithium: Pharmacology, administration, and management of adverse effects – UpToDate [Internet]. [Cited 2021 March 25].
3 Drugs for psychiatric disorders. Treat Guidel Med Lett. 2006;4(46):35-46.
4 Baird-Gunning J, Lea-Henry T, Hoegberg LCG, Gosselin S, Roberts DM. Lithium Poisoning. J Intensive Care Med. 2017;32(4):249-263. doi:10.1177/0885066616651582
5 Lithium poisoning – UpToDate [Internet]. [Cited 2021 March 23]. Available from: https://www-uptodate-com.libproxy.usouthal.edu/contents/lithium-poisoning?search=lithium%20poisoning:%20Rapid%20overview&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1#H23
6 Oakley PW, Whyte IM, Carter GL. Lithium toxicity: an iatrogenic problem in susceptible individuals. Aust N Z J Psychiatry. 2001;35(6):833-840. doi:10.1046/j.1440-1614.2001.00963.x
7 Strobusch AD, Jefferson JW. The checkered history of lithium in medicine. Pharm Hist. 1980;22(2):72-76.
8 Renal toxicity of lithium – UpToDate [Internet]. [Cited 2021 March 23]. Available from: https://www.uptodate.com/contents/renal-toxicity-of-lithium?search=renal%20toxicity%20of%20lithium&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1
9 McKnight RF, Adida M, Budge K, Stockton S, Goodwin GM, Geddes JR. Lithium toxicity profile: a systematic review and meta-analysis. Lancet. 2012;379(9817):721-728. doi:10.1016/S0140-6736(11)61516-X
10 Lazarus JH. Lithium and thyroid. Best Pract Res Clin Endocrinol Metab. 2009;23(6):723-733. doi:10.1016/j.beem.2009.06.002
11 DeBattista C. Antipsychotic Agents & Lithium. In: Katzung BG. Eds. Basic & Clinical Pharmacology, 14e. McGraw-Hill; Accessed April 12, 2021.
12 Ward ME, Musa MN, Bailey LG. Clinical pharmacokinetics of lithium. Journal of Clinical Pharmacology. 1994;34(4):280-285.



