Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Travis Smith, DO; Larry Mellick, MD
Introduction
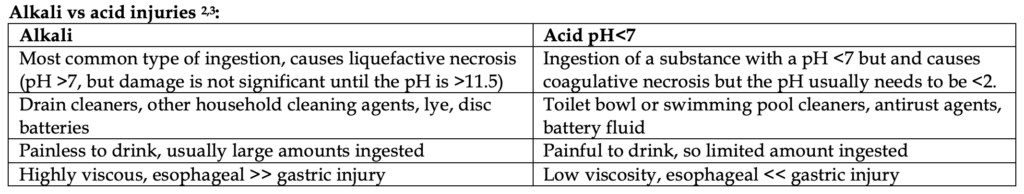
Caustics are agents like bleach or ammonia that can burn or corrode tissue due to strong acid or alkaline nature. They are more common in children (80% of cases) and are usually accidental exposures in children, but in adults, they are unfortunately intentional and often associated with psychiatric illness.1 Adults are more likely to ingest higher amounts of substances as well, resulting in more severe esophageal and gastric damage. Alkaline ingestions are more caustic than acidic ingestions.
Liquid household bleach (5%) is rarely caustic.4 In fact, most standard household detergents, bleaches, and cleaners have pHs 9-11. They rarely cause injuries unless taken in large amounts (>200 mL). This is not true of “pods”, which are more concentrated.5
Presentation
There is a wide variety of how patients present. Unfortunately, early signs and symptoms may not correlate with the severity of tissue damage.6
Patients are usually initially asymptomatic from their injuries. The most common presenting symptom in children is dysphagia. Other symptoms made include oropharyngeal, epigastric, or chest pain, dysphagia, odynophagia, vomiting, hypersalivation, and hematemesis.
Drooling is a foreboding sign and indicates oropharyngeal injury. Hoarseness, stridor, and aphonia are rare, but frighteningly associated with epiglottic or laryngeal injury.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Tachycardia, hypotension, or even fever might indicate esophageal perforation. RED FLAG. See our handout on Boerhaave syndrome for more details on this.
The presence or absence of any clinical symptoms does not predict/exclude the degree of esophageal or gastric injury.
Moreover, don’t just rely on the physical exam. The presence/absence of oral lesions or burns is not a good predictor of esophageal injury.
Complications
Damage to mucosal tissue can lead to irreversible changes like the following complications:
- Bleeding: rare, <3% of patients; manifests in hematemesis after erosion into a vessel.
- Fistulization: can occur any time after massive ingestions.
- Strictures: this is the most common complication, in adults and children. That’s a board question for you. Up to 1/3 of patients with caustic esophageal injury will have strictures. Stricture formation is directly dependent on the depth of injury and occur within 2 months of ingestion.7
- Malignancy: esophageal cancer can occur up to 30% in patients years later.
Workup
Your objective is to distinguish non harmful ingestions from life-threatening ones.
As usual, a general toxicologic workup should occur in the ED, which includes asking EMS or family members about other home medications, as well as other prescription medications found in the household. Make sure to ask and find out the following:
- Specific agent, the amount ingested, time of ingestion, any co-ingestions.
- Contact law enforcement or a family member/loved one to go to the patient’s place of residence to acquire the suspected cleaning agents if the patient is incapacitated or not being forthright.
- Calling the patient’s pharmacy or any helpful EMR retrieving tricks can pay dividends.
Common toxicologic tests to grab include salicylate and acetaminophen level to rule co-ingestions as well as a CBC, CMP, pregnancy test.
Physical Exam
Be attentive to the vital signs as mentioned above. Any patient with stridor, respiratory distress, change in voice, or hoarseness requires laryngoscopy. Early intubation for those in shock and severe respiratory distress is warranted.
Remember that your exam of the oropharynx is limited in its accuracy. You might see edema, erosions, or ulcerations, but this is unlikely. Just because you don’t see anything, doesn’t mean there isn’t damage below your view. Imaging with CT imaging can help assess.
Chest x-ray: perform on all patients. These can rule out other etiologies and might show evidence of esophageal perforation in a minority of patients (e.g., pneumomediastinum, mediastinal widening, subcutaneous emphysema, pleural effusions, hydropneumothorax.
CT neck/chest/abdomen with contrast: This should be performed on all adults with caustic ingestion. CT can reliably show the depth of injury and degree of necrosis and is graded with the following system below8:
- Grade I: Normal-appearing organs
- Grade II: Mucosa is enhanced due to edema, with soft tissue inflammatory change
- Grade III: The absence of postcontrast wall enhancement
Labs are not very helpful and merely help with other toxicologic screening.
Management
Anyone with signs of perforation and/or CT evidence of transmural necrosis in the esophagus or stomach requires emergency laparotomy.9
- Asymptomatic patients without significant ingestion: if the exam is normal and history is non-concerning for large, caustic volume, then the patient can be discharged after they tolerate PO (small glass of water is fine). If the ingestion is in a child, it is recommended that you observe them for “several hours.”
- Symptomatic patients or any with significant ingestion: any symptoms, presence of any oral burns, or history suggesting high-risk ingestion requires hospitalization for endoscopy. Perform laryngoscopy in unstable patients and intubate those with respiratory distress, oropharyngeal or glottic edema. All these patients require ICU admission.
There are no medications or antidotes available. Proton pump inhibitors are used for stress ulcer prophylaxis in those warranting admission. Steroids have not been shown to help, so don’t give them. Broad spectrum antibiotics like ampicillin/sulbactam are only for selected patients with perforation or suspicion for mediastinitis.
An endoscopy is typically performed within the first 24 hours (~3-48 hours).10 It is wise to call GI ahead of time in the ED to assist in arranging this.
Things you should NEVER DO, and you will flunk your boards if you do them:
- Never place an NG tube. It can induce vomiting, therefore worsening esophageal injury and possibly causing perforation.
- Never give emetics like ipecac for the same reasons as above (also activated charcoal does not work).
- Never give neutralizing agents. The damage from the reaction is about instantaneous.11
- Never give steroids. These have not been proven to have any effect.12 There is some debate on whether steroids are helpful in children, but this decision should be made post-EGD and should not be made by the ED physician.
References
- Cheng HT, Cheng CL, Lin CH, et al. Caustic ingestion in adults: the role of endoscopic classification in predicting outcome. BMC Gastroenterol 2008; 8:31.
- Gumaste VV, Dave PB. Ingestion of corrosive substances by adults. Am J Gastroenterol 1992; 87:1.
- Friedman EM. Caustic ingestions and foreign bodies in the aerodigestive tract of children. Pediatr Clin North Am 1989; 36:1403.
- Wasserman RL, Ginsburg CM. Caustic substance injuries. J Pediatr 1985; 107:169.
- Fraser L, Wynne D, Clement WA, et al. Liquid detergent capsule ingestion in children: an increasing trend. Arch Dis Child 2012; 97:1007.
- Gaudreault P, Parent M, McGuigan MA, et al. Predictability of esophageal injury from signs and symptoms: a study of caustic ingestion in 378 children. Pediatrics 1983; 71:767.
- Sarfati E, Gossot D, Assens P, Celerier M. Management of caustic ingestion in adults. Br J Surg 1987; 74:146.
- Keh SM, Onyekwelu N, McManus K, McGuigan J. Corrosive injury to upper gastrointestinal tract: Still a major surgical dilemma. World J Gastroenterol 2006; 12:5223.
- Oakes DD, Sherck JP, Mark JB. Lye ingestion. Clinical patterns and therapeutic implications. J Thorac Cardiovasc Surg 1982; 83:194.
- Poley JW, Steyerberg EW, Kuipers EJ, et al. Ingestion of acid and alkaline agents: outcome and prognostic value of early upper endoscopy. Gastrointest Endosc 2004; 60:372.
- Penner GE. Acid ingestion: toxicology and treatment. Ann Emerg Med 1980; 9:374.
- Chirica M, Bonavina L, Kelly MD, et al. Caustic ingestion. Lancet 2017; 389:2041.
- Gaudreault P, Parent M, McGuigan MA, et al. Predictability of esophageal injury from signs and symptoms: a study of caustic ingestion in 378 children. Pediatrics 1983; 71:767.
- Wason S. The emergency management of caustic ingestions. J Emerg Med 1985; 2:175.
- Bielecki JE, Gupta V. Caustic Ingestions. [Updated 2021 May 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557442/



