Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Larry Mellick, MD
Introduction
An intussusception is a telescoping of part of the intestine into itself. It is the most common abdominal emergency in young children <2 years of age and is the most common cause of bowel obstruction in children. In adults, the diagnosis is rare, and should prompt concern for cancer. The typical age range is 6 to 36 months of age. 90% of patients are within this age range.1 Still, one must consider this diagnosis outside this age range. Those outside the age range are more likely to have a pathologic lead point.
Pathogenesis and Causes
These words are hard to spell, it’s quite annoying.
The most common location involves the ileocecal junction, occurring in 90% of cases.1
Overwhelmingly, 75% of childhood cases are idiopathic with no identifiable masses and no lead point.2
In 25% of cases, there is an underlying pathology that causes a lead point. This is more common in children <3 months old or >5 years old, aka those outside the typical age range.3
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
A lead point is a lesion in the intestine that is trapped by intestinal movement and dragged to a distal segment, precipitating intussusception.4
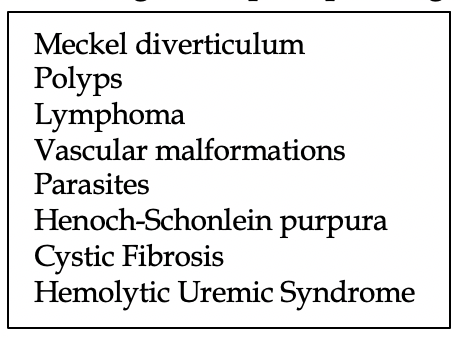
To the right is a table displaying uncommon conditions potentially associated with intussusception.
As the intussusception develops, the mesentery is dragged into the bowel, causing venous and lymphatic congestion with resultant edema.
Viral infections have been implicated as a precipitating cause, but evidence is not definitive.5
Presentation
The classically taught presentation is sudden onset of intermittent, severe abdominal pain.1 These episodes are marked by crying, distress, and occur at 20-minute intervals. In between these episodes the child is said to behave “normally”. Emesis can occur as well. Rarely, a sausage-shaped mass is felt in the right side of the abdomen.
We hate to break it to you, but these symptoms are extremely unreliable. In fact, the triad of pain, palpable sausage-shaped mass, and currant-jelly stool is <15% of patients. Wow that’s poor.6,7
Bloody stool is only seen in 50% of cases, with an additional 25% with occult blood.8
In fact, nearly 20% of infants will not have any obvious distress or pain, and about 30% of patients will not pass any blood in their stool.
Perhaps the least helpful but most common symptom is lethargy, a word that every physician hates. As the pathology progresses, increasing lethargy develops.
To summarize: in any child aged 6 to 36 months of age with isolated and unexplained lethargy or altered consciousness, intussusception should be suspected.
Diagnosis
The history and physical are a wash, but one should still ask about abdominal pain episodes with crying, vomiting, rectal bleeding, and lethargy.
The exam should evaluate for abdominal distention, abdominal masses, and rebound or guarding.
Your differential list in a lethargic infant or toddler with abdominal pain is long, but 3 other diagnoses that also can present with vomiting and bloody diarrhea cannot be missed: malrotation with volvulus, bacterial colitis, and Meckel diverticulum.
Abdominal radiograph with ultrasound should be performed in all suspected cases. No, the radiograph will not diagnose intussusception (only rarely will a target sign be seen on x-ray) but will help rule out perforation and malrotation.
In the hands of an experienced technician, the sensitivity and specificity are 100%, with a NPV of 100% as well.
In other words, a negative ultrasound definitively rules out intussusception.
The classic finding on ultrasound is a “target sign”, which are the layers of intestine within the intestine.
Management
Those acutely ill, unstable vitals, or signs of perforation require surgery.
Other, nonemergent reasons for surgery include if nonoperative reduction is unsuccessful, especially if there is a persistent focal filling defect on imaging concerning for a mass lesion blockage.9
Patients with no perforation will undergo nonoperative reduction via hydrostatic or pneumatic pressure by enema.
Enema reduction has a high success rate (70-85%) yet carries a small risk of perforation (<1%).10, 11 The best part is no sedation or anesthesia is needed for this procedure.
Pneumatic enemas carry a slightly higher rate of success than hydrostatic, but this depends on your institution.12
Success rate of nonoperative intervention is lower in those with delayed presentation, and those with an identifiable lead point.
Important points: no antibiotics are needed in successful cases; they have not been found to be helpful. Diet may be quickly advanced to clear fluids and beyond that if the child tolerates.
Total recurrence rate in successful nonoperative reductions is 10-20%.13 Over 50% of these occur in the first 72 hours, so strict return precautions are recommended. Importantly, recurrence alone is not an indication for surgery.
Asymptomatic intussusception is occasionally discovered during other studies are often managed conservatively, with no attempts at reduction. Spontaneous reductions of these intussusceptions occur frequently. Nevertheless, clear instructions for observation and when to return for further evaluation should be provided to the parents.
Disposition
Patients may be discharged from the ED after a short period (~2 hours) of observation in the ED.
This has been an area of debate, as some have argued that admission and observation is needed. Studies have showed the recurrence rates of intussusception do not differ between children observed at home versus hospital admission.13
We vote for shared decision making with family but aim for discharge home and strict return precautions given to parents.
References
1. Mandeville K, Chien M, Willyerd FA, et al. Intussusception: clinical presentations and imaging characteristics. Pediatr Emerg Care 2012; 28:842.
2. Ntoulia A, Tharakan SJ, Reid JR, Mahboubi S. Failed Intussusception Reduction in Children: Correlation Between Radiologic, Surgical, and Pathologic Findings. AJR Am J Roentgenol 2016; 207:424.
3. Lloyd DA, Kenny SE. The surgical abdomen. In: Pediatric Gastrointestinal Disease: Pathopsychology, Diagnosis, Management, 4th, Walker WA, Goulet O, Kleinman RE, et al (Eds), BC Decker, Ontario 2004. p.604.
4. Lin XK, Xia QZ, Huang XZ, et al. Clinical characteristics of intussusception secondary to pathologic lead points in children: a single-center experience with 65 cases. Pediatr Surg Int 2017; 33:793.
5. Bhisitkul DM, Todd KM, Listernick R. Adenovirus infection and childhood intussusception. Am J Dis Child 1992; 146:1331.
6. West KW, Stephens B, Vane DW, Grosfeld JL. Intussusception: current management in infants and children. Surgery 1987; 102:704.
7. Yamamoto LG, Morita SY, Boychuk RB, et al. Stool appearance in intussusception: assessing the value of the term “currant jelly”. Am J Emerg Med 1997; 15:293.
8. Losek JD, Fiete RL. Intussusception and the diagnostic value of testing stool for occult blood. Am J Emerg Med 1991; 9:1.
9. Pierro A, Donnell SC, Paraskevopoulou C, et al. Indications for laparotomy after hydrostatic reduction for intussusception. J Pediatr Surg 1993; 28:1154.
10. Daneman A, Navarro O. Intussusception. Part 2: An update on the evolution of management. Pediatr Radiol 2004; 34:97.
11. Sadigh G, Zou KH, Razavi SA, et al. Meta-analysis of Air Versus Liquid Enema for Intussusception Reduction in Children. AJR Am J Roentgenol 2015; 205:W542.
12. Beres AL, Baird R. An institutional analysis and systematic review with meta-analysis of pneumatic versus hydrostatic reduction for pediatric intussusception. Surgery 2013; 154:328.
13. Whitehouse JS, Gourlay DM, Winthrop AL, et al. Is it safe to discharge intussusception patients after successful hydrostatic reduction? J Pediatr Surg 2010; 45:1182.