Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Travis Smith, DO
Introduction
For more than 200 years, cardiac glycosides have been used for heart failure due to systolic dysfunction and certain supraventricular tachyarrhythmias. Though its usage has declined, it is still a regularly encountered medication, especially in older patients and those with advanced heart failure, making toxicity a genuine concern. Digoxin toxicity remains a source of morbidity and mortality all emergency physicians should understand. In 2017 alone, there were 1,689 cases of cardiac glycoside exposures reported in the US. 559 had moderate or major toxicity, and 23 died. Additionally, about 1,500 patients were reported to have exposure to cardiac glycoside plant species.
Rare you say? Yes, but boards don’t care. Repeat after us: “you will see digoxin toxicity questions on your boards, and you must be prepared for an oral boards case as well.”
Multiple cardiac glycosides exist in nature, and these were used to treat heart failure before digoxin was manufactured. You should be familiar with their names: foxglove, dogbane, red squill, lily of the valley, oleander, and henbane.
Quick Pathophysiology
In myocytes, the intracellular influx of calcium is necessary for muscle contraction. Cardiac glycosides reversibly inhibit the membrane Na-K ATPase. This increases intracellular sodium and decreases intracellular potassium. The increase in intracellular sodium halts the sodium-calcium channel from expelling calcium from the myocyte. Calcium accumulates inside the myocyte, thus contributing to further contraction.
In summary, cardiac glycosides cause the following:
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
-increased inotropy in cardiac myocytes
-increased vagal tone, reducing conduction from the SA and AV nodes
-shortened repolarization of the atria and ventricles
-decreased refractory period of the myocardium
You can imagine that tinkering with all these cardiac parameters can spell disaster if there is toxicity, and you would be correct.
Too much intracellular calcium can cause after-depolarizations and result in premature beats and triggered arrhythmias.
The decreased refractory period also increases automaticity and heightened risk for arrhythmia.
Let’s focus on digoxin and ignore the plants (#thankgod). Digoxin is the most common cardiac glycoside toxicity. It has a very narrow therapeutic index, so toxicity has a high potential. It is very dependent on the body’s pharmacokinetics.
Normal EKG findings associated with digoxin therapy
We would be remiss to mention the common, expected EKG findings associated with therapeutic digoxin therapy (so-called “digitalis effect”): T wave flattening or inversion, QT interval shortening, and scooped ST segments with depression (Salvador Dali sagging).
Presentation in acute toxicity
Patients typically present bradycardic (increased vagal tone). For the first several hours’ patients might not even have symptoms. EKG findings still might be present early on.
Gastrointestinal symptoms are typically the initial symptoms: n/v, anorexia, generalized abdominal pain.
Later on, neurologic symptoms such as confusion and generalized weakness may be seen. This is due to both direct drug toxicity and cerebral hypoperfusion as well.
Visual changes are rare, but classic on boards. Changes in color vision (chromatopsia), diplopia, photophobia, decreased acuity, or even blindness can occur. Xanthopsia (EM Board Bombs word of the day), is where objects appear yellow. Again, exceedingly rare but boards love it. And no Vincent Van Gough did not suffer from digoxin toxicity despite what you might have heard. Just listen to this discussion from the Curious Clinicians for more.
Out of all objective findings on presentation, arrhythmias are the most common, and virtually any arrhythmia can occur.
The most common arrhythmia: Premature ventricular contractions (PVCs)
The least common arrhythmias: A-flutter, A-fib, and Mobitz type II second degree AV block
Others you need to know: atrial tachyarrhythmias with AV block, VT, V. fib.
Classic test EKG finding: bidirectional ventricular tachycardia (rare, but on boards)
-bidirectional tachycardia is a regular rhythm where every other beat has a different axis as it moves via different conduction pathways.
Workup
As with all suspected poisonings and toxicologic cases, Poison Control should be alerted. Once ABCs are taken care of, you should be asking the following rubric of questions to the patient (if not indisposed), EMS, family, or police:
Agent taken, amount taken, other co-ingestants, time of ingestion.
Most digoxin toxicity cases are accidental, and asking about recent diarrheal illnesses, dehydration, or acute renal insufficiency are good questions because they could hint at reasons the drug levels would suddenly increase in the body.
Fingerstick glucose, EKG, CBC, CMP, salicylate and acetaminophen levels, blood gas, pregnancy test, digoxin level
Digoxin levels should be drawn on presentation and six hours after ingestion.
Electrolyte abnormalities: increase in extracellular potassium is a very common finding.
Hyperkalemia is an important marker and predictor of mortality.
In fact, one study showed patients with a K level >5.5 mEq/L had 0% survival. No patient with a K level <5 died.
Renal injury is commonly seen and is the usual cause of acute toxicity.
Digoxin levels: normal = 0.5 – 0.8 ng/mL (0.65 to 1 nmol/L)
Digoxin levels do not necessarily correlate with toxicity. Treat the patient.
Digoxin levels should not be used to calculate antidote therapy with Fab fragments.
After fab fragments are given, total serum digoxin levels are unreliable because they measure both bound and unbound drug. If available, “free digoxin” levels may be used.
Management
Fab fragments (digoxin-specific antibodies) are the antidote. Empiric treatment is 10 vials of fab fragments for adults, 5 vials for children. Fab fragments may be used for empiric treatment of plant-based cardiac glycoside overdose as well. One vial binds ~0.5 mg of digoxin. Hemodialysis and extracorporeal membrane removal are not effective and should not be used.
When to give fab fragments is fairly obvious:
-Any unstable arrhythmia
-Hyperkalemia
-End organ dysfunction (altered mental status, renal failure)
In general, you should not give fab fragments in an asymptomatic patient that is well-appearing with normal labs just because they have an elevated digoxin level. As always, consult with your toxicologist.
Bradycardia is managed with atropine, hypotension with IV fluids (caution in heart failure patients).
Any unstable tachyarrhythmia in an unstable patient warrants immediate electrical cardioversion. This is not the solution to the problem but every attempt should be made to maintain end-organ perfusion. ACLS guidelines should be referred to.
Hyperkalemia itself does not cause death. Temporizing measures to lower K levels do not reduce mortality. If fab fragments are given, hyperkalemia corrects itself. On the boards, do not treat hyperkalemia.
In practice, we realize these are difficult patients to manage and the K level might return before the digoxin level, prompting the provider to urgently manage an electrolyte issue in the setting of new EKG findings.
However, giving potassium-lowering therapy can actually cause hypokalemia if Fab is given as well which is not good either. In fact, hypokalemia exacerbates digoxin toxicity. Be judicious, do the best you can, and please don’t just “throw meds at the patient hoping something sticks”.
On that note, on the boards, IV calcium should never be given as a preventive measure against hyperkalemia for cardiac protection. There is a dogmatic belief dating back to the 1930s that IV calcium will cause “stone heart”, where the heart enters an irreversible non-contractile state, due to impaired diastolic relaxation. This theory is all hogwash (e.g. foolish). More and more studies suggest there is no evidence IV calcium causes anything serious.
Bottom line: IV calcium is safe to give in patients with digoxin overdose, but it is debatable if it is effective. What we do know: in cases of hyperkalemia where digoxin toxicity has not yet been confirmed, IV calcium is potentially lifesaving and should not be withheld.
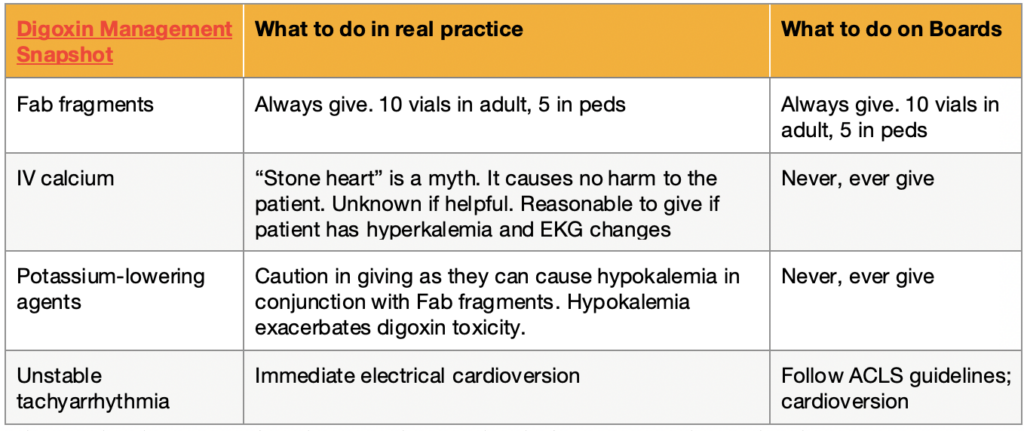
See our table above for a summary of actions to take when it comes to digoxin overdose, both on boards and in practice.
Disposition: all patients should be admitted and monitored a minimum of 72 hours if they received fab fragments. If they are asymptomatic but suspected toxicity is a concern and/or elevated digoxin levels, monitor for 6 hours and repeat level. If repeat is unchanged and patients remain asymptomatic, discharge may be appropriate.
References
1. Eichhorn EJ, Gheorghiade M. Digoxin. Prog Cardiovasc Dis 2002; 44:251.
2. Angraal S, Nuti SV, Masoudi FA, et al. Digoxin Use and Associated Adverse Events Among Older Adults. Am J Med 2019; 132:1191.
3. Gummin DD, Mowry JB, Spyker DA, et al. 2018 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 36th Annual Report. Clin Toxicol (Phila) 2019; 57:1220.
4. Brubacher JR, Lachmanen D, Ravikumar PR, Hoffman RS. Efficacy of digoxin specific Fab fragments (Digibind) in the treatment of toad venom poisoning. Toxicon 1999; 37:931.
5. Botelho AFM, Pierezan F, Soto-Blanco B, Melo MM. A review of cardiac glycosides: Structure, toxicokinetics, clinical signs, diagnosis and antineoplastic potential. Toxicon 2019; 158:63.
6. Ma G, Brady WJ, Pollack M, Chan TC. Electrocardiographic manifestations: digitalis toxicity. J Emerg Med 2001; 20:145.
7. Ribner HS, Plucinski DA, Hsieh AM, et al. Acute effects of digoxin on total systemic vascular resistance in congestive heart failure due to dilated cardiomyopathy: a hemodynamic-hormonal study. Am J Cardiol 1985; 56:896.
8. Lip GY, Metcalfe MJ, Dunn FG. Diagnosis and treatment of digoxin toxicity. Postgrad Med J 1993; 69:337.
9. Cauffield JS, Gums JG, Grauer K. The serum digoxin concentration: ten questions to ask. Am Fam Physician 1997; 56:495.
10. Bhatia SJ. Digitalis toxicity–turning over a new leaf? West J Med 1986; 145:74.
11. Bismuth C, Gaultier M, Conso F, Efthymiou ML. Hyperkalemia in acute digitalis poisoning: prognostic significance and therapeutic implications. Clin Toxicol 1973; 6:153.
12. Eddleston M, Rajapakse S, Rajakanthan, et al. Anti-digoxin Fab fragments in cardiotoxicity induced by ingestion of yellow oleander: a randomised controlled trial. Lancet 2000; 355:967.
13. Li-Saw-Hee FL, Lip GY. Digoxin revisited. QJM 1998; 91:259.
14. DigiFab package insert. Savage Laboratories. Melville, NY 2004.
15. Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS Guideline for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2018; 72:e91.
16. Fenton F, Smally AJ, Laut J. Hyperkalemia and digoxin toxicity in a patient with kidney failure. Ann Emerg Med 1996; 28:440.
17. Van Deusen SK, Birkhahn RH, Gaeta TJ. Treatment of hyperkalemia in a patient with unrecognized digitalis toxicity. J Toxicol Clin Toxicol 2003; 41:373.
18. Levine M, Nikkanen H, Pallin DJ. The effects of intravenous calcium in patients with digoxin toxicity. J Emerg Med 2011; 40:41.



