Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Edan Zitelny, MS4, Blake Briggs, MD
Peer Reviewer: Travis Smith, DO, Sean O’Sullivan, MD
Introduction
Urinary Tract Infections (or UTIs) comprise a broad group encompassing infections of the urethra (urethritis), prostate (prostatitis), bladder/lower urinary tract (cystitis), and infection of the kidney/upper urinary tract (pyelonephritis) (1). Separating the 2 “hemispheres” of the urinary tract will be critical when discussing symptoms, complications, and eventual management of this condition. So buckle up, because we have the “koala-fications” to teach you about infections of down under. We will only focus on UTIs in this document.
Causes and Pathophysiology
A UTI develops following the pathogenic colonization of the vaginal introitus or urethral meatus. These bacteria are often from fecal flora or bacteria introduced by sexual activity. The bacteria ascend via the urethra into the bladder, causing inflammation and, subsequently, the classic UTI symptoms (1). Rarely, pyelonephritis can also be caused by bacteremia.
E. coli, a gram negative encapsulated bacilli, is the most common culprit regardless of location along the urinary tract. This bacteria uses fimbriae to adhere to host cells (1). Its predilection for the urinary tract makes it the most common cause of UTI’s, responsible for upwards of 80-90% of cases (2). There are several other potential causes of UTI’s, with complicated acute cystitis often attributable to either Pseudomonas (healthcare exposures or recent GU instrumentation) or Enterococcus (3). Staph saprophyticus is an occasional cause in healthy young women. We will discuss Proteus and the notorious staghorn calculi below.
Rates of antibiotic resistance of uropathogens have been steadily increasing worldwide, in particular ESBL and carbapenem resistance. Some of the commonly used antibiotics, like ciprofloxacin and TMP-SMX, are a lot less effective now. UTIs with resistance rates approaching 30% in most regions which should leave them as 4th and 5th line options when considering treatment prior to culture reporting.
Several factors are associated with increased risks of UTIs. First and foremost, female gender due to the short length of the urethra. Other risk factors include patients with neurological conditions affecting bladder control and emptying, and anatomic abnormalities affecting the urinary tract or its drainage, male factors include BPH, lack of circumcision, and anal intercourse. (4).
Presentation
Classic symptoms for acute cystitis include dysuria, urinary frequency, urgency, and/or suprapubic pain (5). Hematuria can be seen but is rare as a presenting symptom. If a patient is over 65, the diagnosis may be harder to tease out, with complaints of nocturia, incontinence and lack of well-being hinting toward the diagnosis (5).
Symptoms are probably the best tool we can use to isolate the location of a UTI within the urinary tract. Simple cystitis will not have any systemic symptoms if isolated to the bladder. Conversely, infections ascending beyond the bladder (pyelonephritis) will often show systemic signs like fever, chills, abdominal pain, altered mental status, fatigue, flank pain, and costovertebral angle tenderness. By definition, pyelonephritis is a complex UTI and is treated differently from the simple infection (1).
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
The most important piece of symptomatology are the presence or absence of vaginal symptoms which should direct you to think about other infections rather than just urinary-related.
Importantly, visual clarity/cloudiness of urine, or foul odor cannot be used to rule our or rule in a UTI.
In sexually active females, a pelvic exam may be warranted if symptoms are not convincing for UTI especially in the presence of concerning sexual history.
In males, acute prostatitis is a great mimicker, and there should be a low threshold for rectal examination
In the elderly, nonspecific symptoms such as falls, change in functional status, and even change in mood are NOT reliable indicators of infection, however it is difficult in clinical practice to truly determine which symptoms are or are not relevant to the patient’s acute presentation.
Complications
An episode of acute simple cystitis, while painful, is often a relatively short-lived process. However, some complications may arise that may lead to significant morbidity for patients.
Acute complicated UTI occurs whenever there is a UTI with the following features, which suggests the infection might be spreading into the upper urinary tract: Fever, chills, flank pain, costovertebral angle tenderness
Pyelonephritis is on the end spectrum of acute complicated UTIs.
Myth: all men with acute UTIs are considered complicated infections. This is simply not true. However, any prostatic involvement should be considered in males with urinary symptoms, and we support performing rectal exams on males with urinary symptoms. With that being said, urine cultures should be sent on all males with a UTI.
Who is AT RISK of complicated UTIs including pyelonephritis?
Those with obstructions within the tracts (BPH in males, renal stone, cancer, etc.), anatomic abnormalities, elderly patients, and those with diabetes mellitus.
Patients may present with systemic symptoms, including bacteremia, sepsis, multiple organ system dysfunction, shock, and even acute renal failure (1).
Pyelonephritis may be complicated by progression to more significant sequela. Infection and inflammation of the kidney can lead to various renal abscesses, emphysematous pyelonephritis, and papillary necrosis (1).
Proteus, infections and the presence of staghorn calculi (not be confused with the staghorn fern native to Australia), may be associated with significant morbidity. These struvite stones (classically ammonium magnesium phosphate on board exams) can obstruct the renal medulla and prevent outflow from the kidney, predisposing patients to a rare variant of pyelonephritis known as xanthogranulomatous pyelonephritis. In this condition, there is massive destruction of the kidney by granulomatous tissue, often secondary to obstruction by infected renal stones. Symptoms may last weeks to months and are often insidious and nonspecific (1,5), and may include weight loss, malaise, fever, and anorexia, and a mass may be felt leading to a misdiagnosis of renal carcinoma.
Work-up
For all suspected simple UTI cases, only a urinalysis (UA) should be ordered- it has been shown cultures do not change management in simple cystitis. DO NOT SEND CULTURES on uncomplicated UTIs! DO NOT send a urinalysis on a patient who has an indwelling foley if you are not evaluating them for a UTI (based on other findings like fever, lower abdominal or flank pain). Most all foley catheters are colonized within the first few weeks to 30 days and a culture will almost always be positive. The overtreatment of these patients will ultimately lead to microbial resistance and other antibiotic related complications.
Urine cultures are indicated if there is suspicion of a complicated UTI, the patient is pregnant, male, the patient is a child, or is immunocompromised (including those with diabetes)or the patient is a male. Labs should be sent in complicated UTIs. Blood cultures are not indicated in those who are clinically well appearing, afebrile, and/or planning to be discharged (3). If febrile and/or systemic signs of infection are present, blood cultures should be sent. All females of childbearing age should receive a pregnancy test. We built a table for each component of a UA below so you never feel like you’re lost in the outback:
Urine samples should be a clean catch. We bolded the important stuff in the urinalysis.
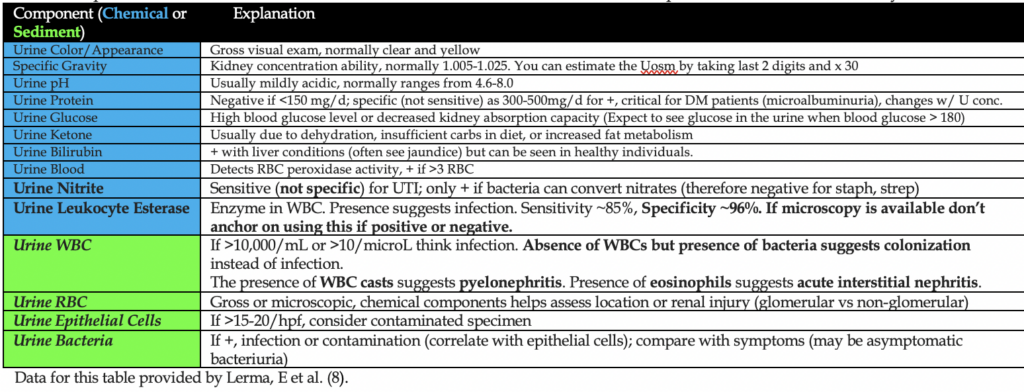
The most important components when diagnosing a UTI specifically are urine WBC, urine leukocyte esterase and urine nitrites. The best accuracy is seen if there are fewer than 5 epithelial cells/hpf. You can see false positive WBCs 6-10/hpf in those with oliguria or dehydration.
A urine WBC > 5 with appropriate symptoms is diagnostic (3). Pyuria is basically a universal finding- its absence suggests an alternative diagnosis.
A positive culture is >10^5 CFU/mL, but there are plenty of reported cases with females having >10^2 CFU/mL, correlate accordingly with symptoms.
Remember that squamous cells suggest a contaminated collection and can give falsely elevated WBCs in the sample.
Who gets CT?
CT abdomen and pelvis without contrast can detect anatomic or physiologic factors associated with acute complicated UTI (as mentioned above). Imaging is not warranted unless the following are present: severe systemic symptoms, any persistent symptoms beyond 48-72 hours with microbial therapy, suspected urinary tract obstruction (decreased urinary output, rise in creatinine).
(See our handout on Kidney Rock: Nephrolithiasis)
CT can show evidence of pyelonephritis (low attenuation and hypodense lesions due to ischemia from neutrophilic infiltration), but it is not sufficiently sensitive or specific to aid in diagnosis.
Treatment
Let’s get this out of the way. Cranberry juice does not prevent UTIs.
The overwhelming majority of cases can be managed as outpatients. In fact, many resolve on their own! The indications for admission would be an inability to tolerate liquids or medications PO or if a patient is presenting as a complicated UTI warranting IV antibiotics, inpatient interventions or general monitoring (6).
Choosing an antibiotic regimen for uncomplicated UTI’s can, ironically, be complicated. You should routinely surf the patient’s medical chart and prior urine cultures. Most commonly, repeat infections are caused by the same organism. Reviewing the sensitivities and specificities using your local antibiogram can help guide antibiotic therapy. Often the initial empiric therapy is nor perfect and culture follow up ensures the best choice of antibiotic.
Uncomplicated UTI:
Nitrofurantoin 100 mg BID 5-7 days. A solid choice for uncomplicated, simple cystitis. Should never be used in those with pyelonephritis or febrile pediatric patients.
3g-Fosfomycin: one-time dose in the ED. Should not be used in pyelonephritis.
Cephalosporins: Increasingly the best option in the ED for uncomplicated and complicated UTIs.
Cephalexin 250-500 every 8 hours for 5-7 days. Does not cover enterococcus.
Cefixime: 8 mg/kg once a day.
Cefaclor: 50-100 mg/kg/day divided into 3 doses.
Cefdinir: 300 mg BID
Stay away from fluoroquinolones- they will work in some patients but are too valuable for other sick patients with many resistant organisms.
Try to avoid Bactrim- higher rates of resistance plus many potential side effects of this sulfa drug in some populations.
Pyelonephritis
Inpatient: Ceftriaxone 1g daily or Piperacillin-Tazobactam 3.375 every 6 hours (preferred if Pseudomonas or other MDR organism is a concern).
Outpatient:
-Cephalosporins (see above section for details)
-Amoxicillin/Clav 875mg BID 10d
-Ciprofloxacin (only in areas of low fluoroquinolone resistance. Try to use the above options first).
References
1. Gupta K, Hooton TM, Naber KG, et al. International clinical practice guidelines for the treatment of acute uncomplicated cystitis and pyelonephritis in women: A 2010 update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clin Infect Dis 2011; 52:e103.
2. NKF. “Urinary Tract Infections.” National Kidney Foundation, 3 Feb. 2017, www.kidney.org/atoz/content/uti.
3. Norris DL, Young JD. UTI. EM Clin N Am. 2008; 26:413-30.
4. Hooton TM, Scholes D, Hughes JP, et al. A prospective study of risk factors for symptomatic urinary tract infection in young women. N Engl J Med 1996; 335:468.
5. Hooton TM. Clinical practice. Uncomplicated urinary tract infection. N Engl J Med 2012; 366:1028.
6. Smithson A, Chico C, Ramos J, et al. Prevalence and risk factors for quinolone resistance among Escherichia coli strains isolated from males with community febrile urinary tract infection. Eur J Clin Microbiol Infect Dis 2012; 31:423.
7. Bent S, Nallamothu BK, Simel DL, et al. Does this woman have an acute uncomplicated urinary tract infection? JAMA 2002; 287:2701.
8. Lerma, Edgar V. “Urinalysis: Reference Range, Interpretation, Collection and Panels.” Edited by Eric B Staros, Urinalysis: Reference Range, Interpretation, Collection and Panels, 4 Mar. 2020, emedicine.medscape.com/article/2074001-overview.
9. LaRocco MT, Franek J, Leibach EK, et al. Effectiveness of Preanalytic Practices on Contamination and Diagnostic Accuracy of Urine Cultures: a Laboratory Medicine Best Practices Systematic Review and Meta-analysis. Clin Microbiol Rev 2016; 29:105.
10. McNeeley SG, Baselski VS, Ryan GM. An evaluation of two rapid bacteriuria screening procedures. Obstet Gynecol 1987; 69:550.
11. Pfaller MA, Koontz FP. Laboratory evaluation of leukocyte esterase and nitrite tests for the detection of bacteriuria. J Clin Microbiol 1985; 21:840.
12. Pappas PG. Laboratory in the diagnosis and management of urinary tract infections. Med Clin North Am 1991; 75:313.
13. Meister L, Morley EJ, Scheer D, Sinert R. History and physical examination plus laboratory testing for the diagnosis of adult female urinary tract infection. Acad Emerg Med 2013; 20:631.
14. Stamm WE. Measurement of pyuria and its relation to bacteriuria. Am J Med 1983; 75:53
15. Wilson ML, Gaido L. Laboratory diagnosis of urinary tract infections in adult patients. Clin Infect Dis 2004; 38:1150.
16. KASS EH. Asymptomatic infections of the urinary tract. Trans Assoc Am Physicians 1956; 69:56
17. Peterson J, Kaul S, Khashab M, et al. A double-blind, randomized comparison of levofloxacin 750 mg once-daily for five days with ciprofloxacin 400/500 mg twice-daily for 10 days for the treatment of complicated urinary tract infections and acute pyelonephritis. Urology 2008; 71:17.
18. Potts L, Cross S, MacLennan WJ, Watt B. A double-blind comparative study of norfloxacin versus placebo in hospitalised elderly patients with asymptomatic bacteriuria. Arch Gerontol Geriatr 1996; 23:153.
19. Dasgupta M, Brymer C, Elsayed S. Treatment of asymptomatic UTI in older delirious medical in-patients: A prospective cohort study. Arch Gerontol Geriatr 2017; 72:127.
20. Sundvall PD, Elm M, Ulleryd P, et al. Interleukin-6 concentrations in the urine and dipstick analyses were related to bacteriuria but not symptoms in the elderly: a cross sectional study of 421 nursing home residents. BMC Geriatr 2014; 14:88.
21. Sundvall PD, Ulleryd P, Gunnarsson RK. Urine culture doubtful in determining etiology of diffuse symptoms among elderly individuals: a cross-sectional study of 32 nursing homes. BMC Fam Pract 2011; 12:36.
22. Petty LA, Vaughn VM, Flanders SA, et al. Risk Factors and Outcomes Associated With Treatment of Asymptomatic Bacteriuria in Hospitalized Patients. JAMA Intern Med 2019.
23. American College of Radiology. ACR Appropriateness Criteria for Acute Pyelonephritis. Last reviewed 2012. https://acsearch.acr.org/docs/69489/Narrative (Accessed on February 27, 2017).


