Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Sam Hopp, MSIII
Peer-Reviewer: Blake Briggs, MD; Travis Smith, DO; Rodney Briggs, MD
Introduction
Preeclampsia is a feared, multisystem condition consisting of hypertension (HTN) and end-organ dysfunction with or without proteinuria in the last half of pregnancy. It can also occur in the immediate postpartum period. 90% of patients present >34 weeks gestational age and have good maternal and fetal outcomes, but the mother and child are still at increased risk for serious morbidity and mortality. 10% of cases present <34 weeks and carry higher risks of preterm birth. Those with preeclampsia have a risk of cardiovascular and renal disease after pregnancy.
In total, hypertensive disorders complicate ~ 10% of pregnancies and are classified into chronic HTN (1%), gestational HTN w/o proteinuria (5-6%), preeclampsia (5%), and eclampsia.1 Being familiar with these conditions is not only important because they will be tested on the written and oral boards, but because they account for over 50,000 maternal deaths and 500,000 fetal deaths worldwide. Let’s start with some basics.
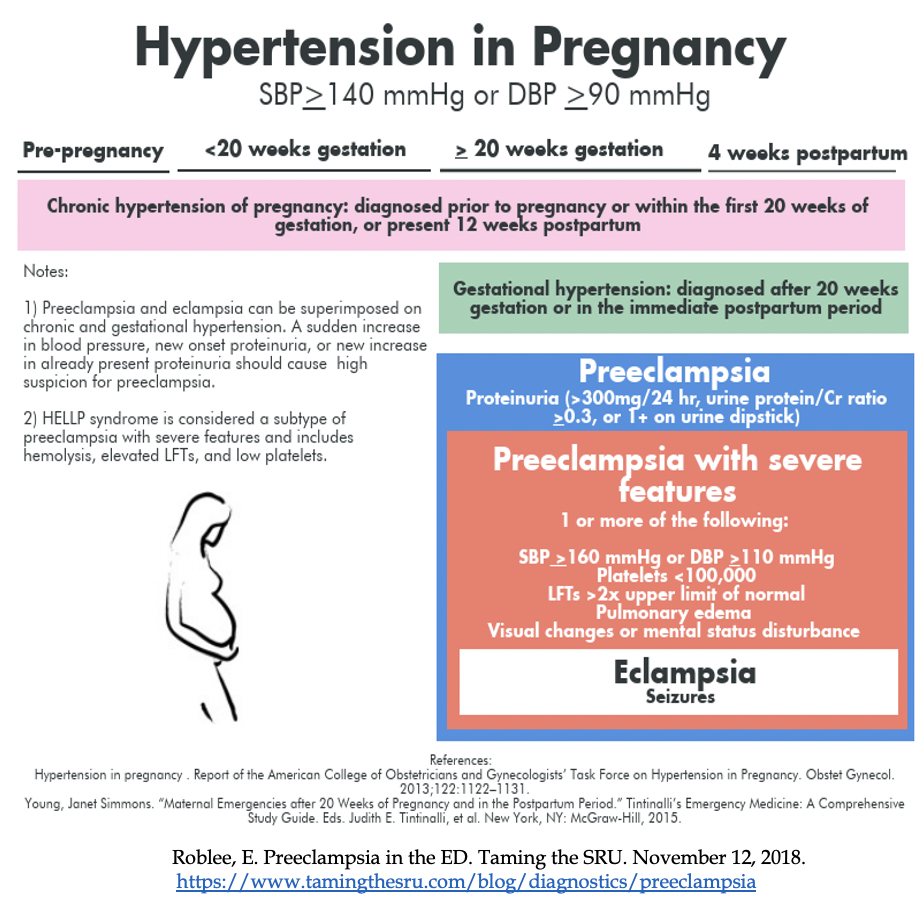
Definitions: These are annoying to remember but easily testable. You must know these definitions to best care for your pregnant patients. In pregnancy, HTN is defined as ≥140 / ≥90. Severe HTN is ≥160 / ≥110.
Chronic HTN of pregnancy: HTN diagnosed before pregnancy or before 20 weeks’ gestation on at least 2 occasions.2 Remember that BP ≥120/80 is abnormal and can be associated with increased risk of preeclampsia.
Gestational HTN: New onset of SBP ≥140 mmHg or DBP ≥90mmHg after 20 weeks’ gestation in a previously normotensive woman on two occasions at least four hours apart or shorter intervals. Blood pressures of >160 / >110 are high risk for risk of severe preeclampsia.2 10-25% of these patients will develop signs and symptoms of preeclampsia.
Preeclampsia: New onset of HTN and proteinuria or new onset HTN and end-organ dysfunction with or without proteinuria after 20 weeks of gestation or postpartum in a previously normotensive woman. 3
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
– ≥ 2+ protein on urine dipstick, proteinuria >0.3 g in 24-hour specimen or protein/creatinine ratio > 0.3
– Platelet count < 100,000
– Serum creatinine > 1.1 or >2x baseline
– Liver transaminases at least 2x upper limit normal
– Pulmonary edema
– New onset and persistent headache not responding to acetaminophen
– Visual symptoms (ex. blurred, flashing lights, sparks, scotomata).3*
– Persistent right upper quadrant or epigastric tenderness, or chest pain
*In rare cases, HTN and proteinuria may be absent, in such cases, any one of the following symptoms may be used to make the diagnosis: thrombocytopenia, renal insufficiency, pulmonary edema, impaired liver function, or new-onset headache with or without visual disturbance.
Preeclampsia with severe features: Preeclampsia with severe HTN and/or specific signs of significant end-organ dysfunction.
HELLP: Variant of preeclampsia with severe features characterized by hypertension plus hemolysis, elevated liver enzymes, and low platelets. HTN is not present in a minority of cases.4
Remember that in normal pregnancy, 30% of women may have dependent foot and ankle edema, but hand and facial edema is concerning.
Eclampsia: Preeclampsia + generalized seizures.5
Mechanism
Largely unknown but many think it is secondary to an acute arthrosis of decidual “spiral” arteries leading to poor placental perfusion and placental ischemia. This then cascades out of control as the hypoxic placental tissue releases all of those bad free radicals to cause oxidative stress, and unchecked “inflammation.” The release of placental antiangiogenic factors into the maternal blood stream causes widespread vascular dysfunction and the clinical presentation of preeclampsia.7
Key Risk Factors: 8
- Past history of preeclampsia (8x higher risk) or history of complications associated with placental insufficiency.
- Pre-existing medical conditions: Pre-gestational diabetes, chronic HTN, autoimmune disorders (lupus, antiphospholipid syndrome), pre-pregnancy obesity w/ BMI >30, chronic kidney disease
- Multifetal pregnancy
- Nulliparity or advanced maternal age (>35)
- African American or Hispanic race (likely due to suboptimal care and screening)
- Family history of preeclampsia
Presentation
85% of affected patients present with new-onset HTN and proteinuria at > 34 weeks of gestation or in labor 10.
10% develop signs and symptoms < 34 weeks 10.
5% can develop signs and symptoms postpartum, which can present as late as 6 weeks post-delivery (don’t forget this pearl).11
“Alarm findings” are signs and symptoms that should raise concern for preeclampsia. 25% of women develop severe hypertension and one of the following symptoms:
– Persistent and/or severe HA
– Visual abnormalities
– Epigastric pain → be careful labeling symptoms as GERD
– Altered mental status
– New dyspnea, orthopnea
– Peripheral edema (Many pregnant women have edema. Any sudden and rapid weight gain >5 lb/week and facial edema are more common in women who develop preeclampsia.)
Remember that when you have HTN in the absence of proteinuria à thrombocytopenia, liver dysfunction, renal insufficiency, pulmonary edema, and cerebral dysfunction are criteria for preeclampsia.
Pearl: All pregnant woman at >20 weeks of gestation or up to 7 days postpartum who present with abdominal pain should be evaluated for HELLP syndrome.
Diagnosis
Preeclampsia is a “can’t miss” diagnosis; it can cause serious consequences for both mother and fetus.
Patients need an accurate blood pressure- manual is preferred.
Labs that you must get include CBC, CMP (liver panels, Cr level), UA/urine protein (protein:Cr ratio in random urine).
– Cr is normally lower in pregnant women, so in preeclampsia it only has to increase by a little (>1.1) to indicate severe disease.
– Hemolysis, coagulopathy issues, transaminitis, and hyperuricemia are also findings.
Assess fetal status – OB/GYN should take care of this. They will perform at a minimum a biophysical profile or nonstress test.
Complications of severe preeclampsia, HELLP syndrome, and eclampsia:
DIC, Spontaneous hepatic and splenic hemorrhage, End-organ failure, Intracranial bleeding, Maternal & fetal death, Abruptio placentae
Treatment for Preeclampsia
Delivery is the ONLY definitive treatment and is indicated in pregnancies > 34 weeks.14 Delivery minimizes the risks of maternal complications and fetal demise.14 If gestational age <34 weeks and there is preterm labor or pre-labor rupture of membranes in the setting of severe preeclampsia are candidates for delivery as well.
HTN management: SBP > 160 mmHg and/or DBP >110 for more than 15 minutes should be treated to reduce maternal complications. Methyldopa is a lame drug- its slow acting and has lupus-like reactions. Forget it.
First line: IV labetalol (rapid onset, good safety profile). 10-20 mg IV push, then 20-80 mg every 20-30 minutes to a maximum dose of 300 mg. Tachycardia is less common and side effects are limited. It is contraindicated in patients with severe asthma or congestive heart failure. 12
Rapid acting oral nifedipine can be used, especially in the absence of IV access. Reflex tachycardia and headaches are common and this agent should not be used long term.13
Refractory hypertension: this is rarely needed, but some experts suggest nicardipine or esmolol infusion.13 However, there are no large RCTs supporting its safety and efficacy in a pregnant patient.
*Remember that all antihypertensive drugs cross the placenta
IV magnesium sulfate to prevent/abort seizures.14 Give 4-6 g IV over 20-min followed by 2 g/hour for at least 24 hours.
The mechanism of magnesium sulfate is not clearly defined, but its primary effect is central. The only contraindication to its use is myasthenia gravis. Caution in those with pulmonary edema. A reduced maintenance dose should be given in renal insufficiency.
There is no consensus on optimal regimen. It is usually initiated to those at the start of labor or induction, or prior to C-section. It should be given to patients not in labor but with severe features.
Expected side effects: diaphoresis, flushing, warmth, vomiting, headache, muscle weakness, visual disturbances, and palpitations. These are NOT reasons to stop the magnesium sulfate infusion.
When to check magnesium levels: seizure while on mag-sulfate, renal insufficiency (every 4-6 hrs), any signs/sx of mag toxicity.
Mag Toxicity = Loss of DTRs (7-10 mEq/L) → respiratory paralysis (10-13 mEq/L) → altered cardiac conduction → cardiac arrest (>25)
Antidote: IV calcium gluconate
Prognosis: Women with preeclampsia are at increased risk of maternal death and obstetric complication. Worldwide, 10% of all maternal deaths are related to preeclampsia. In the US, it is the top 4 leading cause of death.
We appreciate the editorial expertise from Dr. Rodney Briggs. He is board certified in maternal fetal medicine, with over 25 years of experience, including director of MFM at Maricopa Medical Center in Phoenix AZ, Director at Rockford Memorial Hospital in Rockford, IL, and faculty appointments at Northern Illinois University, University of South Carolina, and University of Louisville.
References
1 Hypertension in pregnancy . Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122:1122–1131.
2 Report of the Canadian Hypertension Society Consensus Conference: 1. Definitions, evaluation and classification of hypertensive disorders in pregnancy. Helewa ME, Burrows RF, Smith J, Williams K, Brain P, Rabkin SW. CMAJ. 1997;157(6):715.
3 American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin No. 222: Gestational Hypertension and Preeclampsia. Obstet Gynecol 2020; 135:e237.
4 Diagnosis, controversies, and management of the syndrome of hemolysis, elevated liver enzymes, and low platelet count. Sibai BM. Obstet Gynecol. 2004;103(5 Pt 1):981.
5 Hypertension in pregnancy. Cunningham FG, Lindheimer MD. N Engl J Med. 1992;326(14):927. Department of Obstetrics and Gynecology, University of Texas Southwestern Medical Center, Dallas 75235-9032.
6 Hypertension in pregnancy. Cunningham FG, Lindheimer MD. N Engl J Med. 1992;326(14):927. Department of Obstetrics and Gynecology, University of Texas Southwestern Medical Center, Dallas 75235-9032. 1542342
7 Vascular biology of preeclampsia. Myatt L, Webster RP. J Thromb Haemost. 2009 Mar;7(3):375-84.
8 Risk factors for pre-eclampsia at antenatal booking: systematic review of controlled studies. Duckitt K, Harrington D. BMJ. 2005;330(7491):565. Epub 2005 Mar 2.
9 Screening for Preeclampsia: US Preventive Services Task Force Recommendation Statement. US Preventive Services Task Force, Bibbins-Domingo K, Grossman DC, Curry SJ, Barry MJ, Davidson KW, Doubeni CA, Epling JW Jr, Kemper AR, Krist AH, Kurth AE, Landefeld CS, Mangione CM, Phillips WR, Phipps MG, Silverstein M, Simon MA, Tseng CW. JAMA. 2017;317(16):1661.
10 Hypertension in pregnancy. Cunningham FG, Lindheimer MD. N Engl J Med. 1992;326(14):927. Department of Obstetrics and Gynecology, University of Texas Southwestern Medical Center, Dallas 75235-9032.
11 Postpartum preeclampsia: emergency department presentation and management. Yancey LM, Withers E, Bakes K, Abbott J. J Emerg Med. 2011;40(4):380. Epub 2008 Sep 23.
12 Delayed postpartum preeclampsia and eclampsia: demographics, clinical course, and complications. Al-Safi Z, Imudia AN, Filetti LC, Hobson DT, Bahado-Singh RO, Awonuga AO. Obstet Gynecol. 2011;118(5):1102.
12 A systematic review of nicardipine vs labetalol for the management of hypertensive crises. Peacock WF 4th, Hilleman DE, Levy PD, Rhoney DH, Varon J. Am J Emerg Med. 2012 Jul;30(6):981-93. Epub 2011 Sep 9.
13 ACOG Committee Opinion No. 767: Emergent Therapy for Acute-Onset, Severe Hypertension During Pregnancy and the Postpartum Period.Obstet Gynecol. 2019;133(2):e174.
14 Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 22. Obstet Gynecol. 2020;135(6):e237.
15. Young JS. Maternal Emergencies After 20 Weeks of Pregnancy and in the Peripartum Period. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw-Hill; Accessed May 20, 2021. https://accessmedicine.mhmedical.com/content.aspx?bookid=2353§ionid=219643416



