Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Mary Claire O’Brien, MD
Objectives: define basic types of pacemakers, indications for pacemaker placement, ED evaluation of pacemakers and common complications that are both early and late
Introduction
Pacemaker = its best to think about it just being a generator and leads. The generator creates a pulse, and that pulse travels down the leads into the desired location to have an effect.
Atrial leads = right atrium
Ventricular leads = lay on the posterior or lateral walls of right ventricle
5 letter identification (EM physicians do not need to worry about the last 2 letters):
-first letter → chamber paced/lead location (A = atrial, V= ventricle, D= Dual, O= None)
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
-second letter → chamber being sensed (same letters as above)
-third letter → response of pacemaker to sensed pulse (T = triggered, I = inhibited, D = both, O = none)
Pacemaker settings
Rate: number of pulses generated per minute.
Output/Amplitude: the pulse generated by the pacemaker. These pulses “capture” or initiate depolarization of the paced chamber. Measured in mA. Different hearts require different amounts of output level. If you do not see capture on the monitor, turn up the mA.
Stimulation threshold: minimum output required to repeatedly cause capture. How to find it: turn down the mA until there is no longer capture. Then set the mA to 2-3x that number.
Sensitivity: minimal activity required to detect a native cardiac impulse (P or R wave). Measured in mV. By increasing the sensitivity, you make the pacemaker less sensitive. In other words, the higher the mV, the less sensitive the pacemaker. A great comparison:
Sensitivity is like a fence. The higher the fence, the less the pacemaker “sees” over it. Same with sensing- the higher the number, the less sensing. A lower number means more is sensed.
Asynchronous pacing is coined as sensitivity (mV) being so high that the pacemaker virtually does not detect any underlying rhythm.
Patients usually carry their device cards with them, if not, an overpowered CXR can often show the information. The Pacemaker ID app by Brian Weinrich can identify pacemakers and AICD with pretty darn good accuracy
Indications for pacemaker/AICD placement: sinus node dysfunction (most common reason), cardiac resynchronization therapy in late stage heart failure (usually with EF <20-25%), Mobitz II or 3rd degree AV block, Brugada syndrome, hypertrophic cardiomyopathy, recurrent syncope with asystole, WPW, various prolonged QT syndromes, sustained episodes of VT.
The workup of these patients requires the following diagnostic investigation:
1. Device information
2. Symptoms associated with device malfunction/misfiring
3. Why the device was placed
4. Date of implant and/or most recent repair or interrogation.
Reading pacemaker EKGs:
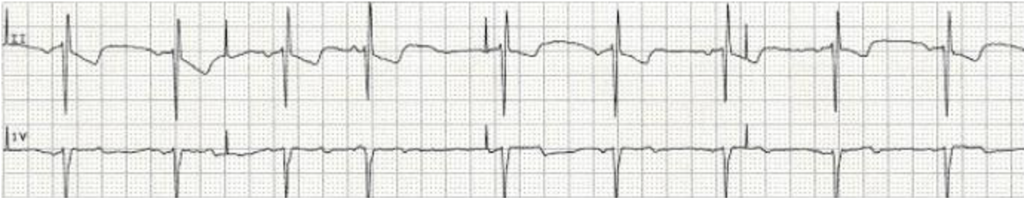
Atrial pacemaker- normal rhythm is easy to identify with pacer spike preceding a narrow QRS.
Ventricular pacemaker- LBBB-like pattern with pacer spikes preceding wide QRS complexes.
Early complications of pacemakers
Recent <6 weeks out from implantation: these are exclusively related to the physical placement of the device itself.
-pocket hematoma, infection, upper extremity DVT, pneumothorax, SVC syndrome
-lead displacement: pacemaker fails to capture or is under-sensing. Patient will have recurrent bradycardia and fatigue. If a ventricular pacemaker, deviation from LBBB is suspicious. Hiccups can suggest deviation to the phrenic nerve.
Late complications
Battery malfunction: rare today thanks to modern pacemaker battery life. Can include palpitations, headaches, fatigue, syncope.
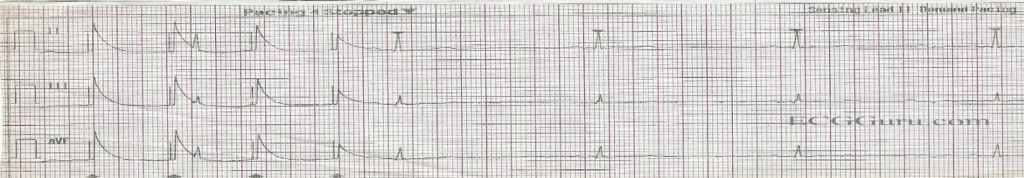
Failure to sense (undersensing): the pacemaker does not detect the patient’s myocardial depolarization. Think “failure to Sense” as the QRS being “Sneaky”. The QRS “sneaks past” the pacer spike. The EKG tracing shows a spike following a QRS complex too early.
Prolonged refractory periods or “blanking” results in failure to recognize a depolarization. Often due to change in voltage of tissue and secondary to changes in patient’s intrinsic EKG complex.
Dangerous! Can lead to ventricular tachycardia.
Most common cause is lead fracture, displacement, or insulation defects. Electrolyte imbalances, myocardial ischemia are other causes.
Actions to take: lower the mV sensitivity level to make the pacemaker more sensitive. Check the battery, check all lead connections.
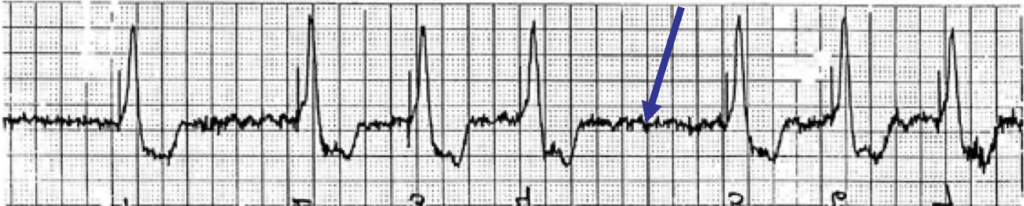
Failure to capture: the heart fails to respond to the pacemaker impulse. On EKG tracing, a pacer spike will appear, but it will not be followed by a QRS complex.
Common causes are similar to above: lead insulation breaks, displacement, fracture. Other causes include myocardial pathology, electrolyte derangement, or antiarrhythmic drug interference.
Types of failure to capture: intermittent (every now and then) versus absolute (never).
Actions to take: Increase the mA. As usual, check the batter, lead connections, and switch pacer box as needed.
Oversensing: pacemaker picks up noise when it shouldn’t. This occurs when electrical signals are inappropriately recognized as native cardiac activity and therefore the pacemaker activity is reduced. Inappropriate signals include large P waves or T waves, skeletal muscle activity, wiring issues.
There can be reduced pacemaker activity if the patient is asked to move their chest or shoulder muscles.
Actions to take: make the pacemaker less sensitive (increase mV). As usual, check the batter, lead connections, and switch pacer box as needed.
Failure to pace: the pacemaker does not generate an electrical impulse. As the name implies, it’s a failed pacemaker so therefore there are no pacing spikes. On an EKG tracing, pacemaker spikes will be missing.
Patients have HR lower than the limit designated by pacemaker. Pacemaker over-sensing is the most common cause.
-Actions to take: check the batteries, switch out the pacer box, check cable connections.
-if not a mechanical problem, adjust settings. Increase output and observe for changes.
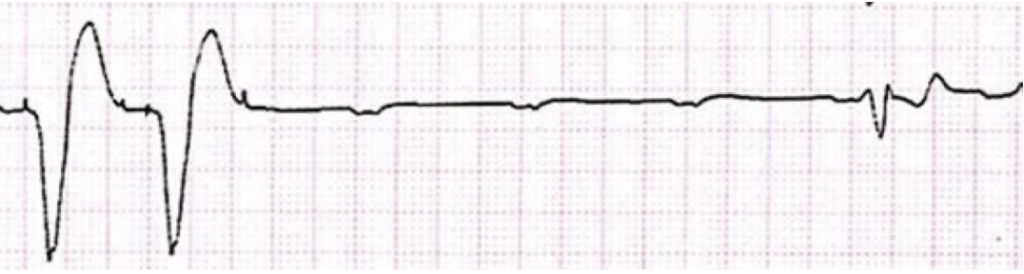
Pacemaker mediated tachycardia: re-entry arrhythmia where the pacemaker itself becomes part of the circuit. The pacemaker becomes the anterograde conduction path, and the AV node is retrograde.
Details of pathophysiology: atrial senses ventricular spike and interprets it as an endogenous atrial depolarization; this triggers another ventricular impulse.
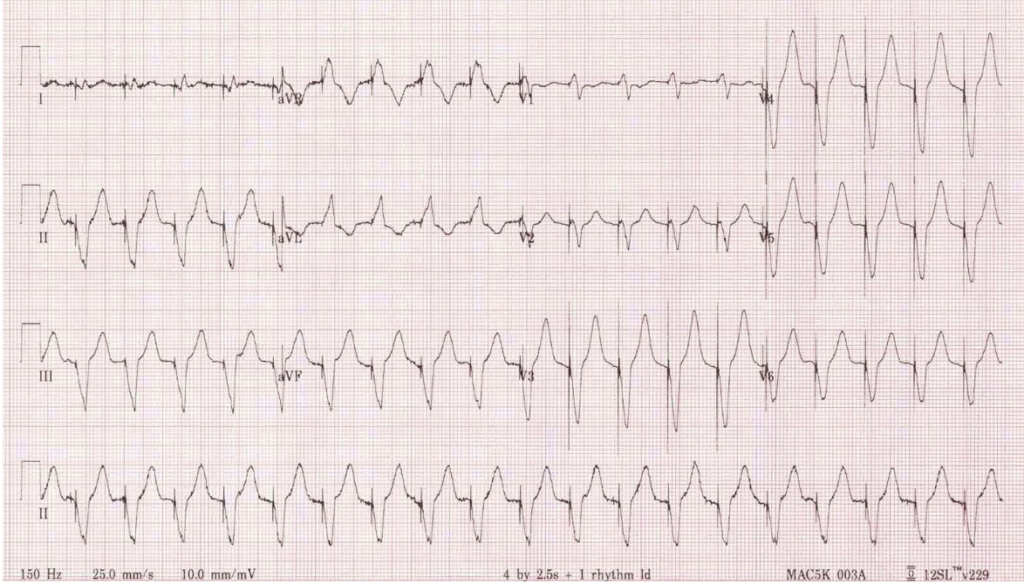
EKG: Rapid wide complex tachycardia (see PDF for EKG photo).
Tx: place a magnet over the pacemaker- it will go to preset asynchronous rate and terminate the anterograde portion of the circuit. Carotid massage, adenosine have both been described with some success as well.
In any of the cases described above, in the event of device failure and hemodynamically unstable, patient may need transcutaneous or transvenous pacing (follow the stable/unstable bradycardia algorithm).
–Pacer pads should be placed 8 cm away from the device if placed.
-Always strongly consider electrolyte abnormalities as a cause
Details of what a magnet does when applied:
Magnet applied to site of pacemaker: Starts asynchronous pacing
Magnet applied to site of ICD: Turns off tachyarrhythmia response function (aka disables it)
This is for MOST DEVICES, there is a fair amount of diversity
References
1. Jacob S et al. Cardiac rhythm device identification algorithm using X-Rays: CaRDIA-X. Heart Rhythm 2011; 8(6): 915-22. PMID: 21220049
2. Kucher N. Deep-vein thrombosis of the upper extremities. NEJM 2011; 364:861. PMID: 21366477
3. Lam CW. Permanent cardiac pacemaker: an emergency perspective. Hong Kong Journal of Emergency Medicine. 2001; 8 (3): 168-175.
4. Martindale J, deSouza IS, et al. Managing Pacemaker-Related Complications and Malfunctions in the Emergency Department. Emergency Medicine Practice. Sept. 2014; 16 (9).
5. Ortega DF. Runaway pacemaker: A forgotten phenomenon? Europace 2005; 7(6): 592-7. PMID: 16216762
6. Riemann JT, Squire B: Implantable Cardiac Devices, in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2010, (Ch) 80: p 1064-75.
7. University of Ottawa Heart Institute. https://www.emboardbombs.com/wp-content/uploads/2023/02/pacing-presentation-notes.pdf



