Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Daniel Phillips, MS4, Blake Briggs, MD
Peer Reviewer: Mary Claire O’Brien, MD
Introduction
Neuroleptic Malignant Syndrome (NMS) is a rare, but life threatening, complication in patients on antipsychotic medications. Prior incidence rates for patients taking antipsychotic agents NMS are ~3%; however, incidence has dropped <1% most likely due to increased awareness over the last decade. Mortality ranges from 3-27%, which is a vast improvement from a 76% mortality in the 1960s.
Causes
NMS is a neurologic emergency associated with neuroleptic (“neuro-depressive”) agents. The pathogenesis of this emergency is largely unknown, however, the medications linked to NMS have dopamine-antagonism in common. Causative anti-dopaminergic medications include 1st generation antipsychotics (most common offenders), 2nd generation antipsychotics, and antiemetic drugs (metoclopramide, promethazine, levosulpiride, etc.).
It is important to note that NMS is an idiosyncratic reaction, not an allergy. This means that (a) it can occur without recent changes in medication or doses and (b) the patient can be restarted on the medications in the future.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Risk factors include high doses of causative meds, recent rapid dose escalation, a change between medications, and parenteral administration. Age and gender are not known to be risk factors.
Presentation
NMS is characterized by a typical tetrad and has progression over 1-3 days (66% patients within 1 week). The tetrad includes:
(1) Altered mental status/delirium/catatonia/stupor (initial symptom in 80% of cases)
(2) Muscle rigidity (“lead pipe”)
(3) Hyperthermia
(4) Autonomic instability
Most patients (70%) have a typical course of symptoms with starting with AMS à rigidity à hyperthermia à autonomic dysfunction. However, there is great variability in the presentation of NMS. The changes in mental status are often underappreciated due to the patient’s psychiatric comorbidities, however agitated delirium or confusion with a change from baseline is a common finding. Muscular rigidity is generalized and extreme, described as “lead pipe rigidity,” meaning that the patient demonstrates stable resistance through all ranges of motion. Here’s a great YouTube clip demonstrating lead pipe rigidity (https://www.youtube.com/watch?v=NQksvNNr07Y).
Hyperthermia with temperatures >38°C are typical, and occasionally temperatures can be >40°C. Autonomic instability manifests as tachycardia, labile/high blood pressures, tachypnea, diffuse diaphoresis, and occasionally dysrhythmias.
Associated lab findings are not diagnostic but can include elevated serum CK, leukocytosis, acute kidney failure.
Diagnosis
There is no diagnostic test for NMS, however it is important to rule out other diseases as well as monitor for complications of NMS. Brain imaging and LP are required to exclude structural intracranial disease & infection. EEG may be done if there is suspicion for to nonconvulsive status epilepticus.
Differential Diagnosis
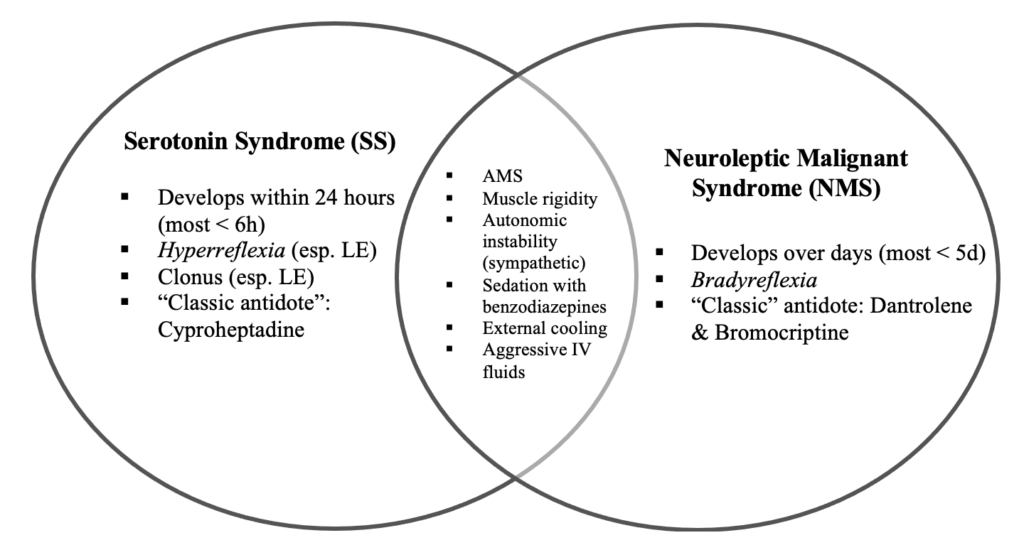
1. Serotonin syndrome – hyperreflexia, myoclonus, nausea/vomiting/diarrhea, more acute in onset, history of serotonergic medication initiation/increased dose.
2. Malignant hyperthermia – similar symptoms (hyperthermia, muscle rigidity, autonomic instability), but more severe and sudden in onset; hx succinylcholine/inhaled anesthetic – think recent intubation and/or surgery.
3. Malignant catatonia – similar symptoms (hyperthermia, muscle rigidity, autonomic instability), includes behavioral prodrome in advance.
4. Other drug-related syndromes (baclofen withdrawal, anticholinergic syndrome, cocaine, ecstasy).
5. Other neurological diseases (CNS infection, seizures, heat stroke, tetanus, pheochromocytoma, etc.).
6. Hyperthyroidism
Complications
Rhabdomyolysis is the most common complication (~30%). Other complications can also occur, such as acute kidney injury, elevated transaminases, cardiomyopathy, dysrhythmias, DIC, and hepatic failure.
Treatment
The first obvious step is to stop all causative agents. Stop giving any antipsychotics, avoid any anti-dopaminergic agents. Aggressive supportive care should be administered in a timely manner to prevent many complications that can be described broadly as “end-organ failure”. Critical care is required, with goals to:
– Lower fever using cooling blankets (note: antipyretic medications do not influence reducing temperature in NMS due to heat production being at level of muscle, not the hypothalamus).
– Lower BP if markedly elevated (best to use pain and sedation medications here).
– Benzodiazepines for agitation (usually 1-2 mg lorazepam per dose). Ketamine is a backup but has never been studied in this population.
What about Dantrolene?
Everyone talks about dantrolene but it’s not the gold standard. However, its often the correct answer on tests. We have been primed since medical school to think of dantrolene because of malignant hyperthermia, which is a rare condition related to mostly anesthetic gasses and succinylcholine.
So, what’s the verdict on dantrolene? It’s debated, and no trials support its use. Start with benzodiazepines in patients suspected of having NMS. Like so many tox and neurologic problems, benzodiazepines should be given for acute agitation. They are also great at muscle relaxation.
Dantrolene can be given but takes longer to get than benzodiazepines (we doubt its stored in the ED). Remember that dantrolene is a powerful muscle relaxant and should never be used in hepatic failure. Bromocriptine is also reported as an agent to give in NMS. It is a dopamine agonist.
Disposition
Psychiatry and Neurology should be called in these patients and may offer insight into their hospital/service protocols, and preferences regarding bromocriptine and dantrolene as well. These patients all require ICU admission.
Prognosis
Most episodes resolve within two weeks with mean recovery times 7-11 days. If no end organ ischemia occurs, most patients recover without neurological sequelae. Mortality rates can be as high as 20%, with the strongest predictors of mortality being disease severity and the occurrence of medical complications. Patients with alcohol/drug addictions were noted to have a higher mortality. Following a drug-free period of two weeks after symptom resolution, antipsychotic medications can be administered with use of a different agent, and care to slowly titrate medication with close monitoring.
Here’s a great Venn diagram distinguishing Serotonin Syndrome vs. NMS:
References:
1. Modi S, Dharaiya D, Schultz L, Varelas P. Neuroleptic Malignant Syndrome: Complications, Outcomes, and Mortality. Neurocrit Care 2016; 24:97.
2. Strawn, J. R., Keck, P. E., & Caroff, S. N. (2007). Neuroleptic Malignant Syndrome. American Journal of Psychiatry, 164(6), 870–876. https://doi.org/10.1176/ajp.2007.164.6.870
3. Keck PE, Pope HG, Cohen BM, McElroy SL, Nierenberg AA. Risk Factors for Neuroleptic Malignant Syndrome: A Case-Control Study. Arch Gen Psychiatry. 1989;46(10):914–918. doi:10.1001/archpsyc.1989.01810100056011
4. Gregorakos, L., Thomaides, T., Stratouli, S. et al. The use of clonidine in the management of autonomic overactivity in neuroleptic malignant syndrome. Clinical Autonomic Research 10, 193–196 (2000). https://doi-org.libproxy.usouthal.edu/10.1007/BF02291355
5. Reulbach, U., Dütsch, C., Biermann, T. et al. Managing an effective treatment for neuroleptic malignant syndrome. Crit Care 11, R4 (2007). https://doi.org/10.1186/cc5148
6. Wu, Y. F., Kan, Y. S., & Yang, C. H. (2011). Neuroleptic malignant syndrome associated with bromocriptine withdrawal in Parkinson’s disease — a case report. General Hospital Psychiatry, 33(3), 301.e7-301.e8. https://doi.org/10.1016/j.genhosppsych.2010.11.013
7. Strawn, J. R., Keck, P. E., & Caroff, S. N. (2007). Neuroleptic Malignant Syndrome. American Journal of Psychiatry, 164(6), 870–876. https://doi.org/10.1176/ajp.2007.164.6.870
8. Velamoor VR. Neuroleptic malignant syndrome. Recognition, prevention and management. Drug Saf. 1998 Jul;19(1):73-82. doi: 10.2165/00002018-199819010-00006. PMID: 9673859.



