Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Azeem Rathore, OMS3
Peer Reviewers: Travis Smith, DO & Blake Briggs, MD
Vertigo links to exam findings: check out Dr. Peter Johns’ Youtube channel for more information. These educational videos are incredible. https://www.youtube.com/channel/UCIt8uVPEbrNXA9dRwQrzdGg
Introduction
Classically defined as “the room is spinning”, vertigo is the illusory of movement. It is a symptom, not a diagnosis. Symptoms arise due to dysfunction of some type to the labyrinth, vestibular nerve, or central structures. It is a common cause of dizziness and is often on the differential with presyncope. It accounts for ~ 4 million visits to EDs nationwide. Vertigo can be a frustrating workup for emergency physicians due to the vague description & usually incongruent and confusing symptoms provided by patients. In fact, it has been shown that 1/2 of patients change the answer to their description of how they feel just minutes apart, so it’s no wonder the differential can range from cerumen impaction to stroke. This is likely because your vestibular system is your 6th sense, literally! Due to the “background functioning” of this special sense, patients are usually unaware of it, & thus have difficulty describing the sensation of dizziness. In this document we provide an overview of common etiologies and discuss what is board relevant. We also provide more clinically relevant ways of asking patients about their symptoms to better uncover the correct diagnosis.
Defining features of all vertigo:
-Worsens with head movement. If symptoms do not worsen with head movement, it’s not vertigo.
-Never continuously lasts for more than a few weeks. Even if chronic lesions are present, the body adapts.
-Dyspnea, palpitations, chest pain, and diaphoresis are NOT suggestive of vertigo and you should consider other causes of dizziness.
Central vs Peripheral Vertigo
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
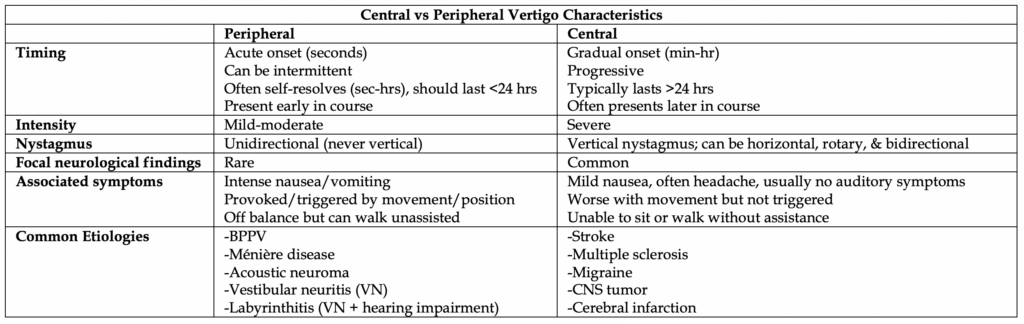
Categorized by either peripheral or central vertigo, physical exam findings are fundamental towards identifying, but be mindful that significant overlap exists. The majority of patients will have a peripheral cause to their vertigo.
History and Physical Exam
– The provider should focus on asking more open-ended questions and categorize the causes of vertigo into peripheral and central. Asking about symptom descriptors is unreliable and can lead the provider astray.
– The sensation of “room spinning” is unreliable. Time course, provoking factors, and aggravating factors are more useful.
– Use the ATTEST history (Associated symptoms, Timing, Triggers, Exam Signs, and Testing) to help stratify the likely syndrome.
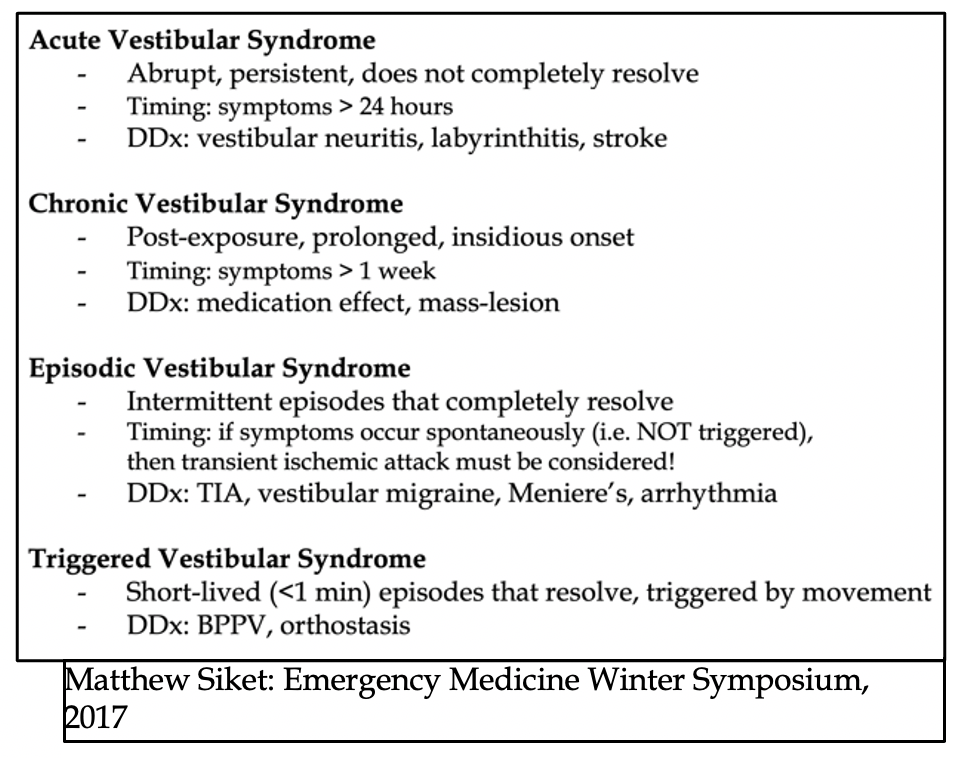
– Abandon the traditional “symptom-quality” approach in favor of a “timing-and-triggers” approach by reorganizing the approach to vertigo into the buckets:
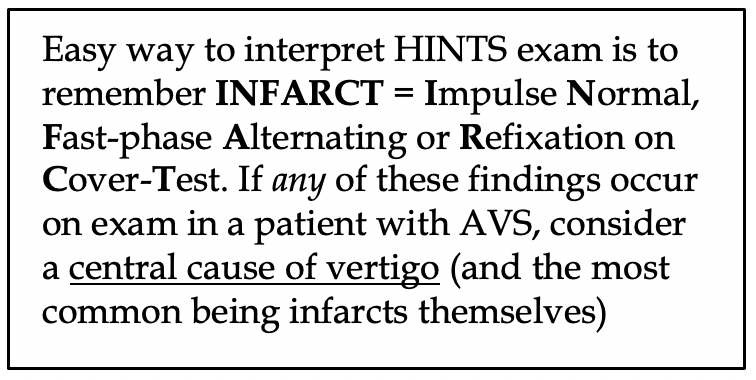
– In suspected AVS, performing a HINTS exam (Head Impulse, Nystagmus, and Test of Skew) may help identify central vertigo. Only patients with persistent ongoing vertigo and spontaneous or gaze-evoked nystagmus should undergo HINTS testing. If any of the three components of the HINTS exam are abnormal, the patient needs admission & neuroimaging. One study showed the HINTS exam outperformed MRI in first 24-48 hours. However, this study was done with neuro-ophthalmologists in a clinic, not EM physicians, so be careful to avoid false positives! DO NOT perform a HINTS exam on patients with EVS or TVS, as they will likely be asymptomatic in the ER (without spontaneous nystagmus or persistent symptoms). For example, if you perform a HINTs exam on a patient with no symptoms, the HINTs exam will suggest a central cause because the head impulse test with be “Normal”.
Unfortunately, there is a lack of major studies looking at the utility of the HINTS. A recent meta-analysis of 5 studies in patients with vertigo was performed with HINTS exam as part of workup and CT or MRI as gold standard. If a neurologist or neuro-ophthalmologist performed the HINTS exam, pooled sensitivity and specificity were 97% and 95%, respectively. If an EM physician or neurologist performed it, 83% and 44% respectively. Ouch. Therefore, be confident in your physical exam skills and make sure you are performing the HINTS on the correct type of patients.
In general, younger patients with acute sustained vertigo symptoms, no neurologic signs, and peripheral symptoms do not need advanced imaging and can expect improvement within a few days’ time.
More on Nystagmus: First, check for spontaneous nystagmus as patients look straight ahead.
◻ Then, test eye movements in all directions to see if nystagmus changes in direction or intensity
◻ It’s named for the fast movement, which moves away from the affected ear/vestibular nerve (e.g. right sided peripheral lesion causes leftward nystagmus (fast movement beating left)
◻ It should never change direction
◻ Usually predominantly in horizontal plane
◻ See video example by clicking the link here
– Bidirectional Nystagmus: direction of nystagmus changes based on direction tested, e.g. left beating nystagmus when looking left, but changes to right beating nystagmus when looking right. Often a sign of stroke. See video example here.
Diagnostics
– If the patient’s story is still unclear, we perform a syncope workup to rule out other non-vertigo causes (EKG, fingerstick glucose, CBC, BMP, urine analysis, B-hCG if applicable).
– The diagnostic yield for head CT ordered in the ER for acute dizziness is poor (2.2%; 1.6% for emergent findings) with low sensitivities for acute ischemic stroke of only around 10%.
– If you chose to image, your money is in the MRI; a negative CT scan DOES NOT rule out badness and sensitivity is only 7-16% in acute phase of stroke. CT also has limited utility for brainstem/cerebellar pathologies due to the overlying skull and bony artifact. MRI changes the diagnosis up to 16% of the time, acutely in 8% of cases.
– MRI still has its own pitfalls: limitations in the posterior fossa whichhas been shown to miss 20% in first 24 hrs, & another 10% in 24-48 hr window. Max sensitivity is at 72-100 hrs.
– Consider CTA/MRA for vascular disease history or concerning presenting for dissection.
Important causes of vertigo
– Posterior canal BPPV: most common type of BPPV. Symptoms triggered by any head or truncal movements. Diagnose with Dix-Hallpike (specific for posterior canal BPPV). Treat with Epley maneuver (click here to see video)
– Horizontal canal BPPV: less common type. Symptoms triggered by horizontal or rotational movements of the head, e.g. rolling over in bed. Diagnose with supine roll test (click here to see video). Treatment similar to Epley, but patient’s head rests on a pillow (rather than hanging from edge of bed) as repositioning maneuver is performed Lempert roll maneuver (see figure 5 in this link).
– Vestibular migraine: Usually episodic, spontaneous symptoms for many years. Strict criteria required:
1) A formal migraine diagnosis by International Headache Society criteria
2) Recurrent episodes of vertigo
3) A migraine symptom during the attack, e.g. headache, photophobia, phonophobia, or aura
4) The exclusion of other causes
– Vestibular neuritis: Acute, benign, self-limited condition presumed to be viral or post-viral. Sadly, less than 50% of patients report a recent viral illness, therefore making it a difficult diagnosis. Dizziness/vertigo is accompanied by N/V, unsteady gait, nystagmus & intolerance to head motion. Usually persists for a day or more. Called labyrinthitis if there is associated hearing loss. PLEASE limit the use of benzodiazepines and/or meclizine to 3 days. Main therapy is early return to activity, ± vestibular exercises, or vestibular rehab/physical therapy.
– Ménière disease: Simultaneous vertigo & cochlear complaints, classic triad of episodic vertigo, sensorineural hearing loss, & tinnitus. Similar to vestibular neuritis, but transient with recurrent episodes lasting 20 minutes to several hours to even a few days. Chronic, conservative therapy includes low salt diet, avoidance of dietary triggers (e.g. caffeine, EtOH). Meclizine is a reasonable medical therapy choice if limited to 3 days; interventional therapy includes intratympanic gentamicin.
– Cerebellar stroke: Symptoms can include dysarthria, dysphagia, dysmetria, limb ataxia (e.g. clumsiness of arms, legs), gait unsteadiness, & vertigo. >80% lack these classic findings & present with isolated vertigo, nausea, vomiting, unsteady gait, & head motion intolerance. Suggestive exam findings: normal head impulse test, abnormal test of skew, inability to sit with arms crossed, inability to walk without support.
Treatment
– Central: symptomatic relief (antiemetics & benzodiazepines); neurology consult, ASA (if ischemic CVA); NSGY (if hemorrhagic CVA) & anticoagulation reversal.
– Peripheral: supportive care with, meclizine, diphenhydramine, promethazine. DO NOT give these meds for more than 72 hrs due to blunting of brain’s ability to ADAPT. Giving these meds for an extended period of time runs the risk of developing chronic vertigo…nobody wants that!
– Tx PEARLS: Use Epley maneuver instead of meds for BPPV – it really does work! Meclizine is not appropriate for treatment of BPPV given the extremely short duration of symptoms. Okay to use meclizine for up to 3 days in acute phase of Ménière, or vestibular neuritis or labyrinthitis. Otherwise you are suppressing normal central re-accommodation & could cause progression to chronic vertigo. Vestibular rehab/exercises: consider use for patient who cannot tolerate Epley maneuver, or for patients with vestibular neuritis.
References
1. Edlow, Jonathan A. “Managing Patients With Acute Episodic Dizziness.” Annals of emergency medicine 72.5 (2018): 602-610.Cole JB, Arens AM, Laes JR, et al. High dose insulin for beta-blocker and calcium channel-blocker poisoning. Am J Emerg Med 2018; 36:1817.
2. Edlow, J. A. “The timing-and-triggers approach to the patient with acute dizziness.” Emergency medicine practice 21.12 (2019): 1-24.
3. Newman-Toker, David E., et al. “Imprecision in patient reports of dizziness symptom quality: a cross-sectional study conducted in an acute care setting.” Mayo Clinic Proceedings. Vol. 82. No. 11. Elsevier, 2007.
4. Goldman, B. “Chapter 164: Vertigo and Dizziness.” Tintinalli JE, Stapczynski JS, Cline DM, et al. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e.
5. Otten, Edward J. “Pocket Emergency Medicine, Richard D. Zane and Joshua M. Kosowsky. Philadelphia, Wolters Kluwer. 2015, 333 pages, paperback, $64.99.” (2015): 1018.
6. Kattah, Jorge C., et al. “HINTS to diagnose stroke in the acute vestibular syndrome: three-step bedside oculomotor examination more sensitive than early MRI diffusion-weighted imaging.” Stroke 40.11 (2009): 3504-3510.
7. Newman-Toker, David E., et al. “Normal head impulse test differentiates acute cerebellar strokes from vestibular neuritis.” Neurology 70.24 Part 2 (2008): 2378-2385.
8. Lawhn-Heath, Buckle C, Christoforidis G. Utility of head CT in the evaluation of vertigo/dizziness in the emergency department. Emerg Radiol (2013) 20:45–49
9. Nelson JA, Viirre E. The clinical differentiation of cerebellar infarction from common vertigo syndromes. West J Emerg Med. 2009;10(4):273–277.
10. Smith T, Rider J, Cen S, et al. Vestibular Neuronitis (Labyrinthitis) [Updated 2019 Dec 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK549866/
11. Ohle R, Montpellier RA, Marchadier V, et al. Can Emergency Physicians Accurately Rule Out a Central Cause of Vertigo Using the HINTS Examination? A Systematic Review and Meta-analysis [published online ahead of print, 2020 Mar 13]. Acad Emerg Med. 2020;10.1111/acem.13960. doi:10.1111/acem.13960
12. Kabra R, Robbie H, Connor SE. Diagnostic yield and impact of MRI for acute ischaemic stroke in patients presenting with dizziness and vertigo. Clin Radiol 2015; 70 (7) 736-742



