Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Travis Smith, DO
As a general rule, it is important to note that when thinking about transfusing anything, a type and screen should be obtained. In a stable patient this is done in order to identify the patient’s ABO blood group and Rh status. Despite there being many other human blood groups that are potentially antigenic, the ABO and Rh type are the ones we are most worried about as the others rarely cause transfusion reactions.
Life threatening: Transfusion associated lung injury (TRALI), Transfusion associated circulatory overload (TACO), Acute hemolytic transfusion reaction, Anaphylaxis, Transfusion associated sepsis
Non-life-threatening: Urticarial reaction, Febrile nonhemolytic reaction, Primary hypotensive reaction
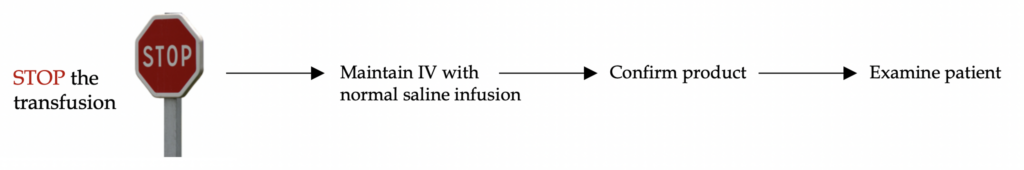
A general approach to all transfusion reactions:
Let’s cover the non-life-threatening reactions first. These are much more common than the life-threatening ones.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Urticarial reaction: A type 1 hypersensitivity reaction (blame the preformed IgE in the recipient). It can occur with any blood product. Results from donor serum proteins reacting with host proteins in some antigen-antibody interaction.
No prophylaxis is needed. Briefly stop the transfusion to give diphenhydramine (steroids not required) and you can restart once symptoms improve and anaphylaxis doesn’t progress. Perhaps the most important aspect of urticarial reactions is ensuring the patient is not experiencing anaphylaxis.
Treatment: symptomatic only; diphenhydramine for itching.
Febrile nonhemolytic reaction: The most common transfusion reaction overall. It is likely due to interleukins and cytokines from donor WBCs.
This is a diagnosis of exclusion, as any fever is concerning for acute hemolytic reaction or transfusion associated sepsis (extremely rare in the US). Follow your hospital policy when a fever develops (this protocol likely differs). It most likely will involve stopping transfusion and returning the unit to the blood bank for analysis. If symptoms have stabilized and the unit is deemed okay then the transfusion can be restarted.
No prophylaxis is needed, but patients will need leukoreduction for future transfusions.
Treatment: symptomatic, Tylenol for fever.
Primary hypotensive reaction: unknown etiology, but patient’s blood pressure (systolic, diastolic, or both) will drop 30 mmHg or more at some point during the infusion and immediately return to normal when the infusion is completed.
The problem with this diagnosis is that it is even less common than the life-threatening ones. So, if a patient’s BP drops during transfusion, you should be concerned about the scary diagnoses like hemolytic reaction, transfusion associated sepsis, and TRALI.
Treatment: monitor closely, if BP remains in acceptable range continue transfusion.
Next let’s examine the life-threatening reactions. In general, severe reactions present within 15 minutes of infusion, so stay vigilant early on. Thankfully these reaction are becoming less and less common in the US. TRALI had been the leading cause of transfusion-associated mortality up until 2016 when the most common cause of death was 🌮 TACO.
TRALI: traditionally the most common cause of death from transfusion reactions. One of the mechanisms involves the association with female multiparous donors which suggests a mechanism of passive transfer of antibodies (anti-leukocyte) in the transfused blood product, with subsequent activation of recipient white blood cells.. Since 2009, > 90% of blood banks have incorporated that of a male-only, malepredominant, or never-pregnant female plasma donating policy to limit this reaction.
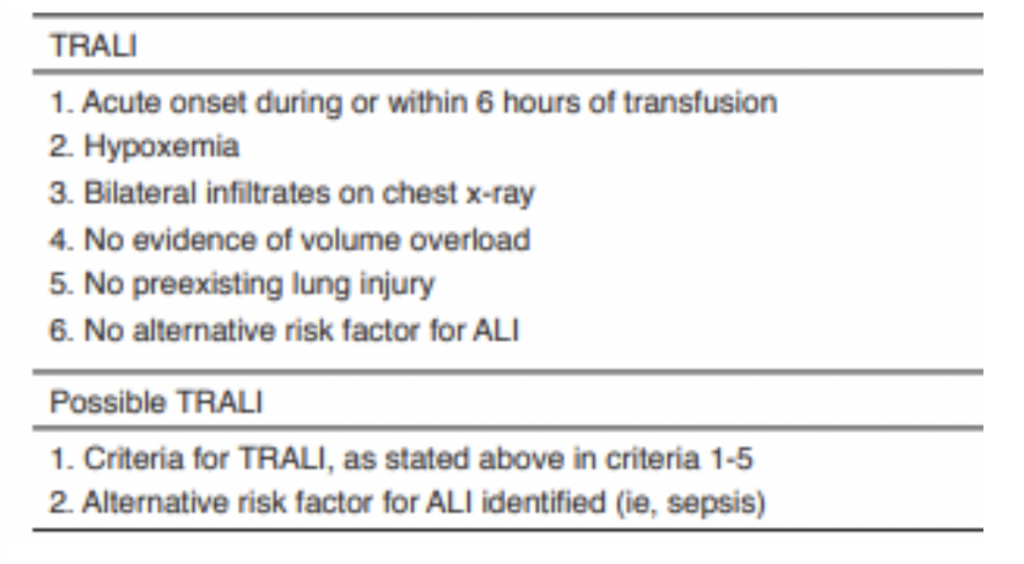
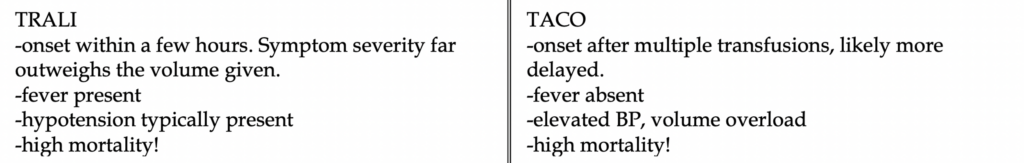
Dx: requires five criteria to be met (see table below) It presents within hours of infusion. These patients present with fever, respiratory distress, and hypotension.
Treatment: supportive. Supplemental oxygen, NIPPV, possibly intubation.
TACO 🌮: about as common as TRALI with an incidence ranging from 0.1-1% depending on the cohort of patients. It is caused by circulatory overload from the transfusions, usually of higher volume or those in the extremes of age. Recipients typically have an underlying cardiovascular history and positive fluid balance. Patients present several hours after multiple transfusions with elevated blood pressure and possibly flash pulmonary edema.
Expect BNP to be elevated as the BNP ratio of > 1.5 had a specificity of nearly 90%.
Treatment: supplemental oxygen, diuretics, NIPPV. Rarely intubation is required.
Determining TRALI vs TACO:
In real life, this can be difficult. Thankfully, the treatment plans are quite similar.
Acute hemolytic transfusion reaction: the most feared reaction, thankfully rare. Its presentation is usually immediate, but can be delayed up to 2 hrs. It is triggered by a few millimeters of blood due to an ABO mismatch. Pre-formed host antibodies destroy donor RBCs.
Fever is the #1 symptom, followed by chills, hypotension, flank pain, and classically oozing from the IV site (#scary).
Treatment: stop transfusion (most fatalities are associated with transfusion > 200 mL of blood). Immediately give IV normal saline at high speed. The goal is to “dilute” the hemoglobin in the blood and minimize its coming into contact with host antibodies. Emergency hemodialysis might be needed if massive hemolysis and resultant hyperkalemia occur.
Anaphylaxis: Rapid onset of anaphylactic shock, with 2 or more of the following: hypotension, respiratory distress, wheezing, urticaria, or GI symptoms.
Classically is due to IgA deficiency but also can have a haptoglobin deficiency.
Treatment: same as every anaphylaxis. IM Epinephrine! All the other drugs are secondary (diphenhydramine, H2-blocker, steroids).
See our handout “Beware the Bees: Guide to Anaphylaxis” on the website for more details on managing anaphylaxis.
Transfusion associated sepsis: rare. Fever is the most common presenting symptom. Pay close attention to the blood products, they could have a purple/brown hue and platelets can have excessive bubbles present (#sketchy).
Workup
Stabilization of the patient should occur simultaneously, but labs can help separate certain emergencies from each other as well as from non-life-threatening causes. All patients with suspected acute hemolytic transfusion reaction, anaphylaxis, sepsis, and TRALI will require labs and chest x-ray.
CBC with differential, CMP, coagulation studies, LDH, haptoglobin, repeat ABO testing with additional antibody tests, blood cultures, lactate.
Parting thoughts
If your patient has a fever when receiving a transfusion, think of these on your differential:
TRALI, febrile hemolytic transfusion reaction, sepsis, febrile nonhemolytic transfusion reaction (the latter is a diagnosis of exclusion).
If a patient is in respiratory distress, think of these: TRALI, anaphylaxis, TACO.
If the patient has a subjective fever but no actual elevated temperature, wait 15-30 minutes and restart transfusion if patient remains asymptomatic otherwise.
References
1. Hume HA, Popovsky MA, Benson K, et al. Hypotensive reactions: a previously uncharacterized complication of platelet transfusion? Transfusion 1996; 36:904.
2. AABB Technical Manual, 17th, Roback JD, Grossman BJ, Harris T, et al (Eds), American Association of Blood Banks Press, Bethesda, MD 2011. P.237.
3. Metcalf RA, Bakhtary S, Goodnough LT, Andrews J. Clinical Pattern in Hypotensive Transfusion Reactions. Anesth Analg 2016; 123:268.
4. Skeate RC, Eastlund T. Distinguishing between transfusion related acute lung injury and transfusion associated circulatory overload. Curr Opin Hematol 2007; 14:682.
5. Fatalities Reported to FDA Following Blood Collection and Transfusion Annual Summary for FY2016. https://www.fda.gov/media/111226/download
Scott K, Greineder, C, Conlon, LW. “The Use Of Blood Products In The Critically Ill Patient: Indications And Risks.” EB Medicine. January 24, 204. Assessed June 21, 2020. https://www.ebmedicine.net/topics.php?paction=showTopic&topic_id=394