Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Introduction
It seems straightforward right? Swollen joint, painful and warm to touch, recent onset- tap it. Sounds easy, but it is often missed by providers. Why? Many think that septic arthritis is something other than septic arthritis, like rheumatoid arthritis, local trauma, or crystal-induced arthritis. That’s bad form.
Bacteria are by far the most common cause. Less common causes of infection in the joint vicinity include septic bursitis, Lyme disease, or certain viruses (e.g. Cikungunya, Dengue, Zika). In those with history of foreign travel or immunocompromised folks, don’t forget about fungi and mycobacteria.
Risk factors
For organisms to enter a joint space, one of the following is needed:
1) Direct inoculation: bacterial spread from the outside environment directly into the joint capsule. Think penetrating trauma, recent surgery or instrumentation, or, rarely, intraarticular injection.
2) Hematogenous spread: Much more common. Organisms spread from the bloodstream. This is classically bacteremia, and we associate 2 major risk factors with this situation:
a. Patient’s joint integrity is weak/damaged to begin with: preexisting joint disease (i.e. crystal arthritis, RA, osteoarthritis), age >50, any joint hardware present.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
b. Systemic risk factors: diabetes mellitus, IV drug abuse, alcoholism, indwelling catheters.
3) Contiguous spread from nearby deep space infection such as osteomyelitis. This is the least common method.
Combining any of these risks substantially increases one’s chances of developing septic arthritis.
Pathophysiology
There is no basement membrane in the synovial space, so therefore once bacteria penetrate the joint capsule, it’s like a jailbreak and they seed the entire cavity.
Causative organisms: both on exams and “real life”, joint infections are classically monomicrobial.
Staphylococcus aureus: by far the most common cause of septic arthritis. Otherwise known as Darth Vader, the dark lord of rheumatologic and dermatologic infections.
Streptococcus species: classically pneumoniae or pygones.
Neisseria gonorrhoeae: most common cause of septic arthritis in sexually active, young patients. On the test they will be <30 years old.
Overall, gonococcal arthritis makes up <2% of all gonorrhea complications. It’s rare, but it’s also hard to diagnose. The triad of tenosynovitis, dermatitis, and polyarthralgias occur frequently. The arthritis tends to be migratory, which is both unique and classic for this disease. Synovial cultures are only positive in 50% of cases along with a low bacterial count, so nuclear amplification tests are preferred. Make sure to not only do arthroscopy but get cervical/urethral samples as well.
Check out our Podcast Episode 56 on gonococcal arthritis, “Tinder Swipe for Gonorrhea”
Brucellosis: zoonotic infection that is a gram-negative coccobacillus. Infection comes from unpasteurized milk or cheese, or direct contact with an infected animal.
Borrelia burgdorferi: Lyme disease. Suspect in those that meet epidemiologic criteria (outdoors in a high-risk area, erythema migrans rash, fever, migratory arthralgias).
Check out our podcast episode 25 on lyme disease, “Doxycycline for all, #blessed”
IV drug abuse or immunosuppression: Pseudomonas makes an appearance, but honestly who knows what bug is causing the infection in these patients. Almost any bacteria, fungi, or even mycobacteria could be an issue.
Penetrating trauma to the joint: think polymicrobial, anaerobes, and the usual skin flora.
Presentation: classically monoarticular, large joints are the most common sites, and the knee is involved >50% of cases. Patients will present with fevers, joint pain, swelling, warmth, and limited range of motion (all these symptoms are seen in 80% of patients). In ~20% of patients, 2-3 joints could be involved. Polyarticular infections are more common in those with RA, Neisseria gonorrhoeae infection, or overwhelming sepsis.
If you see axial joint involvement, immediately think IV drug abuse history.
Younger patients can be febrile, older patients might have a more insidious presentation.
Diagnosis: Clinical suspicion is important, as the blood work is of limited helpfulness.
Blood cultures are only positive in about 50% of cases. The WBC count, ESR, CRP are commonly ordered and can be elevated, but are nonspecific.
X-rays should be performed, especially if recent manipulation or surgery of the join occurred.
Ultrasound is more sensitive for effusions than x-rays.
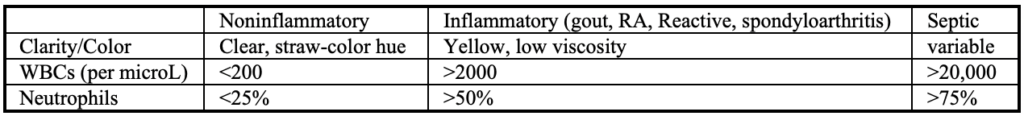
The real money is in the bedside arthrocentesis. It needs to be performed prior to antibiotic administration. Certain joints require radiographic guidance (i.e. hip or sacroiliac).
Send the synovial fluid for gram stain, culture, WBC count with differential, crystal assessment with polarizing microscope.
Key findings:
· >20,000 WBCs with mostly neutrophils = strongly supportive of septic arthritis in the correct clinical context
· Gram stain is only positive in 30-50%
· Synovial fluid culture is positive in >60% of patients with nongonococcal arthritis
Cultures are no help in most cases due to the organisms being S. aureus, but in rare cases they might grow strange, less common organisms.
Cultures suck for N. gonorrhoeae, so nucleic acid amplification is preferred.
If the effusion is hemorrhagic, trauma is the most common cause, followed by coagulopathy or neoplasm.
Differential diagnoses
-Traumatic arthritis: bloody synovial fluid, history of trauma)
-RA: symmetric, RA usually mimics septic arthritis and can be very difficult to tease out one or the other).
-Gout or pseudogout: history of prior attacks, often first metatarsal joint location, tophi, crystals on synovial fluid. Look for crystals, BUT if crystals are positive and gram stain is positive, the patient can have both! Treat for both!
-Reactive arthritis: GI or GU symptoms, conjunctivitis, or skin lesions
Treatment
Drain the joint. You can do this during the initial arthrocentesis and your patient will thank you for it. Consider a septic joint as an abscess!
Who needs surgery? When drainage not achieved by bedside, penetrating trauma with residual foreign body, joint effusion persists days after aspiration.
Antibiotic selection
Gram positive suspected: start with Vancomycin → if MSSA use cefazolin, nafcillin, oxacillin
→ if MRSA, vancomycin, daptomycin, linezolid, clindamycin
Gram negative suspected: ceftriaxone, cefotaxime, ceftazidime, cefepime
The initial antibiotic regimen should be tailored to culture and susceptibility results when available.
Time course: for patients with septic arthritis due to S. aureus in the setting of concomitant bacteremia (but no evidence of endocarditis), IV therapy for four weeks is preferred. In general, no matter the cause, most studies agree on four weeks total of therapy.
Prognosis
One study showed 3% mortality. It causes higher morbidity than people think, mainly for older patients and with comorbidities. In one study, polyarticular septic arthritis had a mortality rate up to 50%!
In one study with 121 septic arthritis cases, a “poor joint outcome” (amputation, arthrodesis, prosthetic surgery, or severe functional deterioration) was found in 1/3 of patients. Again, the biggest adverse prognostic factors were old age and pre-existing joint disease.
IV drug abuse patients with septic arthritis are high risk for morbidity, and it’s getting more common. In one nation-wide series of septic knees, patients with injection drug user-related septic arthritis increased from 5% in 2000 to 11% in 2013.
References
1. Margaretten ME, Kohlwes J, Moore D, Bent S. Does this adult patient have septic arthritis? JAMA 2007; 297:1478.
2. Mathews CJ, Coakley G. Septic arthritis: current diagnostic and therapeutic algorithm. Curr Opin Rheumatol 2008; 20:457.
3. Kaandorp CJ, Krijnen P, Moens HJ, et al. The outcome of bacterial arthritis: a prospective community-based study. Arthritis Rheum 1997; 40:884.
4. Goldenberg DL. Septic arthritis and other infections of rheumatologic significance. Rheum Dis Clin North Am 1991; 17:149.
5. Goldenberg DL, Reed JI. Bacterial arthritis. N Engl J Med 1985; 312:764.
6. Mor A, Mitnick HJ, Greene JB, et al. Relapsing oligoarticular septic arthritis during etanercept treatment of rheumatoid arthritis. J Clin Rheumatol 2006; 12:87.
7. Nadarajah K, Pritchard C. Listeria monocytogenes septic arthritis in a patient treated with etanercept for rheumatoid arthritis. J Clin Rheumatol 2005; 11:120.
8. Schett G, Herak P, Graninger W, et al. Listeria-associated arthritis in a patient undergoing etanercept therapy: case report and review of the literature. J Clin Microbiol 2005; 43:2537.
9. Katsarolis I, Tsiodras S, Panagopoulos P, et al. Septic arthritis due to Salmonella enteritidis associated with infliximab use. Scand J Infect Dis 2005; 37:304.
10. McBride S, Mowbray J, Caughey W, et al. Epidemiology, Management, and Outcomes of Large and Small Native Joint Septic Arthritis in Adults. Clin Infect Dis 2020; 70:271.
11. Morgan DS, Fisher D, Merianos A, Currie BJ. An 18 year clinical review of septic arthritis from tropical Australia. Epidemiol Infect 1996; 117:423.
12. Xu C, Peng H, Li R, et al. Risk factors and clinical characteristics of deep knee infection in patients with intra-articular injections: A matched retrospective cohort analysis. Semin Arthritis Rheum 2018; 47:911.
13. Ross JJ, Saltzman CL, Carling P, Shapiro DS. Pneumococcal septic arthritis: review of 190 cases. Clin Infect Dis 2003; 36:319.
14. Allison DC, Holtom PD, Patzakis MJ, Zalavras CG. Microbiology of bone and joint infections in injecting drug abusers. Clin Orthop Relat Res 2010; 468:2107.
15. Mikhail IS, Alarcón GS. Nongonococcal bacterial arthritis. Rheum Dis Clin North Am 1993; 19:311.
16. Zhao J, Zhang S, Zhang L, et al. Serum procalcitonin levels as a diagnostic marker for septic arthritis: A meta-analysis. Am J Emerg Med 2017; 35:1166.
17. Liu C, Bayer A, Cosgrove SE, et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children. Clin Infect Dis 2011; 52:e18.