Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewers: Mary Claire O’Brien, MD, Travis Smith, DO
Introduction
Everyone knows diabetes predisposes to so many pathologies. Perhaps one of the more substantial sources of morbidity and mortality are foot infections. The greatest risk factor for diabetic foot infections (DFIs) is neuropathy, followed by peripheral vascular disease. Other contributing factors include autonomic neuropathy which decreases sweating, resulting in dry skin with entryways for bacteria. Concomitant peripheral arterial disease impairs blood flow to the extremities. The greatest risk for neuropathy is poorly controlled hyperglycemia. Patients are slow to recognize ulcers and subsequent infections due to decreased sensation in their lower extremities and minor trauma usually goes unrecognized. In this review we will cover the presentation, diagnosis, and antibiotic choices for diabetic foot infections.
Microbiology
Polymicrobial infections are most common. The deeper the infection, the stranger it gets in terms of organisms.
Superficial wounds (look like cellulitis): think usual monomicrobial skin flora, Streptococcus and Staphylococcus groups, with MRSA being a major concern. Deep, chronically infected, previously treated: polymicrobial with bad bugs, Pseudomonas, Enterococcus, Enterobacteriaceae.
Wounds that look necrotic, gangrenous with concurrent systemic toxicity: think polymicrobial with the above organisms, plus sprinkle in some anaerobes like anaerobic strep (Peptostreptococcus), Bacteriodes and Clostridium.
It is important to investigate underlying patient risk factors, like recent hospitalizations, prior abx use, prior cultures, or residence in a long-term care facility. This can key you into those at risk for MRSA, ESBL, Pseudomonas, or vancomycin-intermediate S. aureus infections.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Presentation
Cardinal signs of inflammation are helpful but not present in all cases. Due to peripheral arterial disease, warmth and erythema may not be relied upon. Vital sign abnormalities such as fever, tachycardia, or hypotension are uncommon (especially the latter), but their presence is strongly suggestive of infection.
Due to decreased sensation, diabetics are less likely to complain of pain. Infections have a higher risk of progression to deeper tissues as a result. These deeper infections will manifest with bullae, crepitus on palpation, skin discoloration, foul odor, and purpura which suggest a necrotizing infection needing emergent management (do not wait on labs or imaging, call a surgeon and start broad spectrum antibiotics!).
Osteomyelitis is a feared, relatively common complication of these untreated wounds. The worst part about it is that it can occur without evidence of local soft tissue infection. Sneaky, sneaky!
Clinical risks associated with osteomyelitis: wounds >2 cm2, exposed bone or ability to probe to bone, “sausage” toe digits (erythema and edema of the digits), or chronic nonhealing wounds over bony prominences.
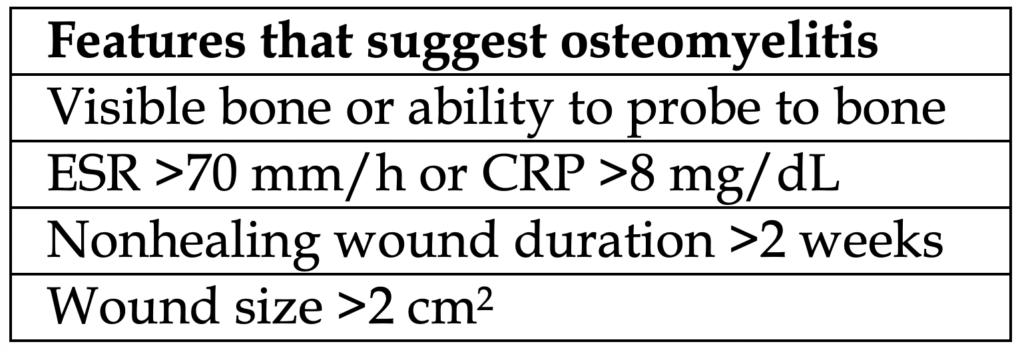
ESR and CRP are routinely sighted as screening labs for osteomyelitis. If ESR >70 mm/h and CRP >8 mg/dL increase the probability, however these are neither highly sensitive nor specific for osteomyelitis.
Bottom line: if you are concerned, order them, but they are not at all definitive in diagnosing osteomyelitis.
Diagnosis
Thorough history detailing how long the wound has been there, history of prior infections, recent trauma, other associated signs/symptoms. The exam is the most thorough foot exam you’ll do in medicine. Test for sensation and vascular insufficiency (ABI <0.9) throughout the foot and compare to the other. Look extensively for ulcers and wounds, making sure to move the digits, evaluating the web spaces and under skin creases. Tinea pedis causes skin breakdown in the web spaces and will need to be treated too.
If you suspect a deep wound, probe it and check if it goes to bone. X-rays of the foot are a good imaging start. Also remember that diabetics do not recall trauma when in actuality they have fractures. If there is an overlying wound that can be a nidus for infection. Other things to evaluate on x-ray: foreign bodies or gas in soft tissue.
X-ray findings suggestive of osteomyelitis: cortical erosion, periosteal reaction, mixed lucency, or sclerosis. Overall, x-rays have a poor sensitivity of around 43-75% with a specificity of 75-83%.
Labs are the usual: electrolyte and chemistry panels, CBC, and CRP, ESR. Often, inflammatory markers are indeterminant, especially with early of infection. In combination with imaging, labs might hint toward osteomyelitis as a cause.
In cases where osteomyelitis is unclear but is still a concern, MRI can be ordered, but this should not delay antibiotics and admission. In x-rays where osteomyelitis is clearly evident, MRI is unnecessary and likely will not change management.
Clinical Pearl: Many foot wounds are colonized by bacteria, so a positive wound culture in the absence of inflammatory findings does not mean infection!
There are no clearly defined criteria for diagnosing diabetic ulcers.
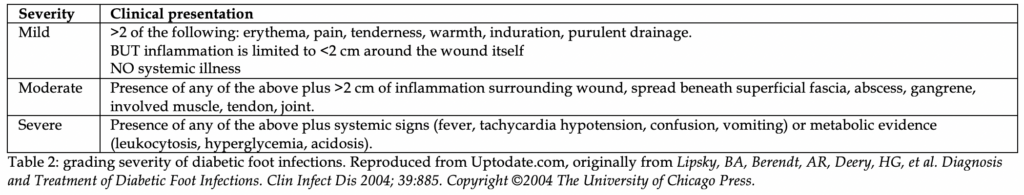
In general, >2 of the following are enough: erythema, warmth, tenderness, swelling, induration, purulent drainage. A summary of the grading scale developed by the Infectious Diseases Society of America (IDSA) in 2004 is below. It has prognostic value, with moderate and severe grading having a higher rate of amputation, higher level of amputation, and increased admission to the hospital. Stay tuned for a more updated table in a few years. Right now, there is really no clinical or prognostic different between moderate and severe, so their difference in this table is purely academic.
Management
Good nutrition, glycemic control, wound care, and antibiotics are the core tenets of diabetic foot infections. Admission is not always required but think about the number of diabetics who can be discharged from the ED and are able to complete all the above tenets. We usually err on the side of admission for most mild infections and we admit all patients with wounds moderate or severe (Table 2).
Wound care includes debridement of calluses and dead tissue, as this is a nidus for infection. Relieving pressure from the foot wound is essential as well. Any necrosis, deep abscesses, or gangrene should prompt surgical evaluation.
Wound cultures are often over-ordered and not helpful as these patients are colonized with bacteria to begin with.
When should you get wound cultures? Moderate or severe wound infections and when there is concern for multidrug resistant organisms.
How you should obtain wound cultures: swab the purulent discharge from the wound or curettage the wound base following a superficial debridement. Superficial wound swabs alone are not helpful and unreliable. In osteomyelitis, bone biopsy is preferred. Orthopedics is usually consulted for this during admission.
Antibiotic therapy details
This is based on wound severity (Table 2 above).
For mild infections: your usual coverage of Staph and Strep. If no history of MRSA or suspicion is low given the presentation and a “first time” occurrence, cephalexin, amoxicillin-clavulanate, or clindamycin is fine.
For MRSA coverage: clindamycin (~50-75% MRSA coverage), trimethoprim-sulfamethoxazole, % doxycycline (both with (>90% MRSA coverage). For moderate to severe infections, including concern for osteomyelitis: need to cover Staph and Strep again, but also worry about anaerobes and sometimes Pseudomonas.
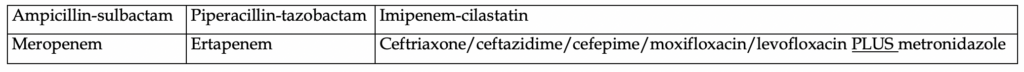
MRSA concern in moderate to severe infections? Add on either Vancomycin, Linezolid, or Daptomycin
What covers Pseudomonas? Piperacillin-tazobactam, imipenem-cilastatin, meropenem, high-dose ceftazidime (2g), cefepime, ciprofloxacin (variable), levofloxacin (variable).
Duration of therapy: depends on severity, depends on wound care needs, depends if there is osteomyelitis. In general, 1-2 weeks if no osteomyelitis, and after there is evidence the infection has resolved and all appropriate wound care has occurred.
References- please refer to this document’s page on website for complete list of references.