Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Introduction: Anaphylaxis is a sudden, systemic-wide mast-cell degeneration resulting in life-threatening distributive shock. It is underreported and undertreated. Lifetime prevalence is 2% in the US, and this has been increasing in recent years. Prompt diagnosis is essential, as death can occur in minutes.1 Anaphylaxis is most responsive to treatment in its early phases, delayed anaphylaxis is associated with higher mortality.2
Presentation
The median time interval from symptom onset to arrest is 5 minutes in iatrogenic causes, 15 minutes from insect-venom, and 30 minutes from food-based causes.1Anaphylaxis has an extremely unpredictable course depending on the patient’s allergen type and frequency of exposure, as well as the overall health of the patient. It is impossible and dangerous to predict how rapid it will progress, or how severe it will become.3
The key to diagnosing and treating anaphylaxis is quickly recognizing the criteria and not relying on “accessary” medications. Epinephrine should primarily be given and is the only agent that reduces mortality.
Most common cause in children: foods > medications. In adults: medications > foods
Risk factors: those with cardiovascular disease, COPD, asthma, chronic beta-blocker, or ACEI users.
Limited history: this should NOT delay treatment with epinephrine! Known allergies? Change in medications? What is the likely exposure and how long ago since last exposure? Has this happened before?
Limited physical exam: examine skin for rash/swelling, examine face/neck for angioedema, listen for wheezing/stridor. 20% of presenting patients do not have a rash.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Criteria for anaphylaxis- only ONE of these has to be present to nail the diagnosis
1) Acute onset <6 hours with skin findings and either respiratory symptoms or hypotension.
2) 2 or more of the following after likely exposure to a known allergen: skin findings, respiratory symptoms, hypotension, GI symptoms (vomiting, epigastric pain)
3) Hypotension after likely exposure to a known allergen.
Often many healthcare providers do not suspect anaphylaxis in the absence of hypotension but as shown above this does not have to be present! See Figure 1 for an overview of the high yield critical actions of anaphylaxis management.
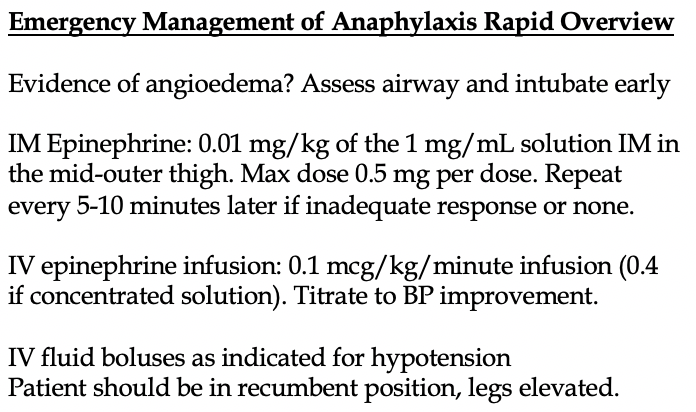
Danger signs: respiratory distress +/- stridor. Look for evidence of facial, tongue, voice alteration, or oral edema. This is concerning for angioedema and should prompt intubation. Strongly consider awake intubation with flexible scope. In a minority of cases, cricothyroidotomy may be required when there is severe enough airway edema.
Treatment: 0.01 mg/kg IM Epinephrine for patients of ANY age, with a max dose 0.5 mg per single dose. Epinephrine is the only drug that addresses all the pathologic components of anaphylaxis.
The dose should be drawn up using a single 1 mL syringe using the 1 mg/mL formulation of epinephrine (“anaphylactic epinephrine”). It should be injected into the outer thigh. None of the other medications discussed below are as important as epinephrine. No formal study has ever proven epinephrine’s efficacy versus placebo (for obvious ethical reasons), but it is clear that it has clinical benefit.
Do not give anaphylactic-dosed epinephrine SQ, do not give IV.4,5 That is not correct. The former will have an erratic onset, the latter may harm the patient. In short, IM dosing of epinephrine is faster and safer with less cardiac complications.
More and more, the ratio labelling way of describing epinephrine dosing (1:1000 vs 1:10000) has fallen by the wayside. Ampules of 1 mg/mL were labelled as 1:1000, but this caused medication errors and iatrogenic harm to the patient. Since 2016, these labels have been removed from many epinephrine labels.6
When an autoinjector is available, use this instead to avoid dose calculation, errors, and delays in administration/
Infants and children 10 to 25 kg should receive 0.15 mg by autoinjector.7
Patients >25 kg should receive 0.3 mg by autoinjector.8
IM epinephrine may need to be repeated in 5–10-minute intervals if there is no response or unsatisfactory response. Up to ~35% of patients will need a second dose.9
Be prepared to switch to an IV infusion early, and if a patient is requiring a second dose, be ready to initiate the drip early and avoid delays.
IV epinephrine
Avoid boluses in most cases, there are significantly higher rates of iatrogenic cardiac complications and dosing errors.10
If you are waiting for your IV infusion to begin and the patient is in extremis, push-dose epinephrine can be your friend. Push 0.5 to 1 mL (50-100 mcg) of push-dose epinephrine from a 10 mL syringe as needed every 5-10 minutes.
To make a typical solution, mix your epinephrine drip by adding the entire 10 mL contents of a 0.1 mg/mL prefilled “cardiac epinephrine” syringe (total of 1 mg) to a 1000 mL bag of saline. This results in 1 mcg/mL solution and delivers 1 mcg/minute for each 60 mL/hour of solution given.
Start the infusion at 0.1 mcg/kg/minute (range: 0.05 to 0.2 mcg). Increase the infusion rate every 2-3 minutes by 0.05 mcg until the BP improves by at least 10%.
We prefer the concentrated solution, great for patients who are already receiving a lot of IV fluids. To make a concentrated solution, mix your epinephrine drip by adding the entire 10 mL contents of a 0.1 mg/mL prefilled “cardiac epinephrine” syringe (total of 1 mg) to a 250 mL bag of saline. This results in 4 mcg/mL solution and delivers 1 mcg/minute for each 15 mL/hour of solution given.
Start the infusion at 0.4 mcg/kg/minute (range: 0.05 to 0.2 mcg). Increase the infusion rate every 2-3 minutes by 0.2 mcg until the BP improves by at least 10%.
Adverse effects of epinephrine
There are no absolute contraindications to its usage, but common side effects include mild anxiety, restlessness, palpitations, and headaches. Very rarely, ventricular arrhythmias may occur. IV boluses, especially if incorrectly given, carry the highest risk.11
There is theoretical risk of worse adverse effects in those with cardiac disease, but the risk of anaphylaxis is much higher and studied.
IV fluids
Expect massive fluid shifts. Anaphylaxis is a form of distributive shock. Within minutes, up to 35% of a patient’s intravascular volume can move to the extravascular space due to severe vascular permeability.12
IV fluids should be used in concert with epinephrine for management of hypotension.
Still hypotensive?
If the patient is still hypotensive after maximum epinephrine IV infusion dose and IV boluses, there is some anecdotal evidence for vasopressin as a second line agent. Honestly, use whatever vasopressor you want here- norepinephrine is fine too.
Vasopressin dose: 1-5mg IV bolus followed by infusion of 1-5mg/hr.
Glucagon
Patients on beta-blockers or ACEI are at higher risk of severe anaphylaxis.13 Interestingly, one retrospective study showed that 789 patients on beta-blockers with anaphylaxis had no increased epinephrine dosing than those not on beta-blockers.14
However, if a patient does appear to be refractory to beta-blockers, glucagon can be given 1-5 mg IV, followed by an infusion.15 Remember that glucagon can cause vomiting!
Adjunctive agents
None of these reduce mortality or relieve airway obstruction caused by anaphylaxis. You can give them to reduce symptoms, but that is it. H1 blockers (cetirizine 10 mg or diphenhydramine 25 mg IV), H2 blockers (famotidine 10 mg IV).
It is suggested that administration of an H1 blocker might decrease progression to anaphylaxis, but this was a retrospective study.16 In short, you can give these medications with minimal harm, but never let them take precedence over epinephrine.
No more steroids?
Glucocorticoids (methylprednisone 1-2 mg/kg) are given to “prevent” recurrence of anaphylaxis, yet their evidence is lacking. One study of 220 patients failed to show benefit of preventing a biphasic reaction.17 We do not administer glucocorticoids in patients who respond well with epinephrine and are discharged from the ED. If patients are being hospitalized and/or have bronchospasm from asthma, they have a role.
Disposition
All patients require observation until complete symptom resolution. No one agrees on the exact time of observation needed for those who are successfully treated.
Biphasic reactions, or anaphylaxis that occurs hours later, is extremely rare.18 It appears to be greatest in patients who had severe anaphylaxis (hypotension, multiple doses of epinephrine needed).17
So, admit any resolved patients who suffered from severe anaphylaxis for overnight observation.
Observe all the others for 2-3 hours (no evidence basis), and discharge with an autoinjector prescription with instructions on its usage. Don’t forget the last step. In one study of 1885 patients, ~30% did not receive a prescription.
References
1. Pumphrey RS. Lessons for management of anaphylaxis from a study of fatal reactions. Clin Exp Allergy 2000; 30:1144.
2. Simons KJ, Simons FE. Epinephrine and its use in anaphylaxis: current issues. Curr Opin Allergy Clin Immunol 2010; 10:354.
3. Simons FE. Anaphylaxis, killer allergy: long-term management in the community. J Allergy Clin Immunol 2006; 117:367.
4. Simons FE, Gu X, Simons KJ. Epinephrine absorption in adults: intramuscular versus subcutaneous injection. J Allergy ClinImmunol 2001; 108:871.
5. Simons FE, Roberts JR, Gu X, Simons KJ. Epinephrine absorption in children with a history of anaphylaxis. J Allergy Clin Immunol 1998; 101:33.
6. https://www.fda.gov/drugs/information-drug-class/single-entity-injectable-drug-products (Accessed on June 19, 2020).
7. Halbrich M, Mack DP, Carr S, et al. CSACI position statement: epinephrine auto-injectors and children < 15 kg. Allergy Asthma Clin Immunol 2015; 11:20.
8. Sicherer SH, Simons FER, SECTION ON ALLERGY AND IMMUNOLOGY. Epinephrine for First-aid Management of Anaphylaxis. Pediatrics 2017; 139.
9. Korenblat P, Lundie MJ, Dankner RE, Day JH. A retrospective study of epinephrine administration for anaphylaxis: how many doses are needed? Allergy Asthma Proc 1999; 20:383.
10. Campbell RL, Bellolio MF, Knutson BD, et al. Epinephrine in anaphylaxis: higher risk of cardiovascular complications and overdose after administration of intravenous bolus epinephrine compared with intramuscular epinephrine. J Allergy Clin Immunol Pract 2015; 3:76.
11. McLean-Tooke AP, Bethune CA, Fay AC, Spickett GP. Adrenaline in the treatment of anaphylaxis: what is the evidence? BMJ 2003; 327:1332.
12. Brown SG, Blackman KE, Stenlake V, Heddle RJ. Insect sting anaphylaxis; prospective evaluation of treatment with intravenous adrenaline and volume resuscitation. Emerg Med J 2004; 21:149.
13. Nassiri M, Babina M, Dölle S, et al. Ramipril and metoprolol intake aggravate human and murine anaphylaxis: evidence for direct mast cell priming. J Allergy Clin Immunol 2015; 135:491.
14. White JL, Greger KC, Lee S, et al. Patients Taking β-Blockers Do Not Require Increased Doses of Epinephrine for Anaphylaxis. J Allergy Clin Immunol Pract 2018; 6:1553.
15. Thomas M, Crawford I. Best evidence topic report. Glucagon infusion in refractory anaphylactic shock in patients on beta-blockers. Emerg Med J 2005; 22:272.
16. Kawano T, Scheuermeyer FX, Gibo K, Stenstrom R, Rowe B, Grafstein E, Grunau B. H1-antihistamines Reduce Progression to Anaphylaxis Among Emergency Department Patients With Allergic Reactions. Acad Emerg Med. 2017 Jun;24(6):733-741.
17. Shaker MS, Wallace DV, Golden DBK, et al. Anaphylaxis-a 2020 practice parameter update, systematic review, and Grading of Recommendations, Assessment, Development and Evaluation (GRADE) analysis. J Allergy Clin Immunol 2020; 145:1082.
18. Pourmand A, Robinson C, Syed W, Mazer-Amirshahi M. Biphasic anaphylaxis: A review of the literature and implications for emergency management. Am J Emerg Med 2018; 36:1480.