Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Travis Smith, D.O.
Introduction
The pericardium is a loose fibroelastic sac covering the epicardium that is made up of visceral and parietal layers. it acts to prevent friction from occurring during each heartbeat by providing lubrication. There is usually up to around 50 ml of pericardial fluid which allows the heart to pump out about 5 L per minute (average cardiac output). Any inflammation or too much fluid accumulation, however, can constrict the heart’s ability to contract and relax. Acute pericarditis is the most common cause of pericardial disease as is seen in about 0.2% of hospitalized patients.1 This document will review the causes, diagnosis, and management of pericarditis.
Clinical presentation
Despite medical school teaching, acute pericarditis presents in a variety of ways. Here’s how it’s traditionally taught:2,3
· Patient history of recent viral syndrome.
· The hallmark is chest pain that is sharp, pleuritic, and improved by sitting up and leaning forward.
· A friction rub may be auscultated on exam (like two pieces of paper rubbing together).
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
· EKG changes with widespread, diffuse ST elevation.
In reality, it is rarely a perfect picture. Let’s dive into the details.
Chest pain: >95% of patients have it.4 As noted above, its sharp, retrosternal, and improves with leaning forward. But in reality, clinicians are not the best at diagnosing causes of chest pain by symptomatology and exam alone (only 70% accurate for cardiac etiology in one recent study), so patients can certainly present with variations in their chest pain description, making it very difficult to distinguish it from other causes of chest pain.5
It usually develops fairly suddenly, located over the anterior chest with radiation to the left trapezial ridge (due to inflammation of the joining diaphragmatic pleura). Of note, when uremia is a cause of pericarditis, chest pain is rarely present.
Friction rub: if present, it’s the most common exam finding and is highly specific for pericarditis. Its intensity waxes and wanes over hours, and it is best heard with the diaphragm of the stethoscope over the left sternal border.6 The sensitivity varies, and no solid studies are available. In one small study of 100 patients, a rub was heard in 85%.7 In another study, it was found to be 35%.4 Your guess is as good as ours.
Questions you should ask are of the usual “chest pain” variety and should be aimed at looking for a cause of the pericarditis: a history of cardiac disease, recent MI, autoimmune disorders, or prior malignancy.
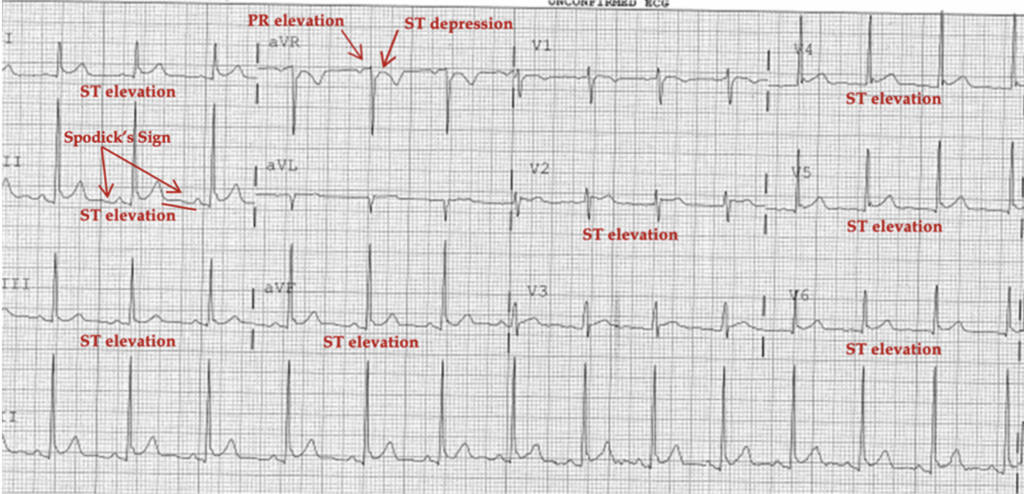
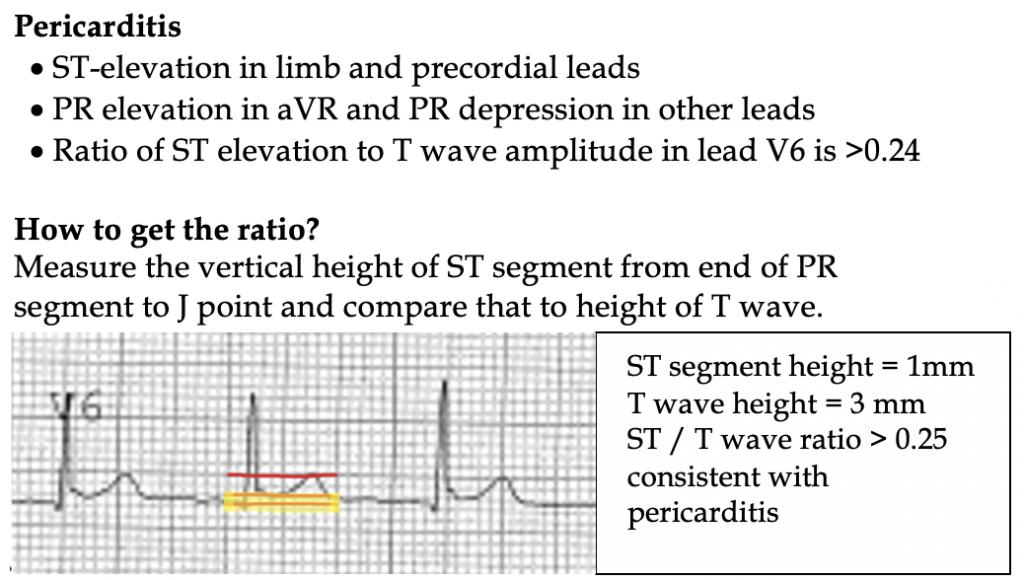
The EKG is one of the core features in diagnosing pericarditis. Unfortunately, it changes often during the disease course and goes through multiple “stages” of findings over the course of several weeks.
Stage 1– hours to days. Classic widespread ST elevation (more pronounced in lateral precordial leads) and PR depression in I, II, III, and aVF with solitary reciprocal depression in leads aVR and V1.
Stage 2– normalization of ST and PR segments but still can be elevated.
Stage 3– widespread T wave inversions.
Stage 4– normalization of the EKG.
In reality, it is highly variable and rare that patients will go through this traditional path EKG changes, but you probably need to be familiar with it for the boards. Indeed, atypical EKG changes are seen in up to 40% of pericarditis patients!4
What we do know is that arrhythmias are virtually unheard of in acute pericarditis if the patient does not have underlying heart disease. If arrhythmias are present, you need to think about pericarditis’ evil cousin, myocarditis, see hour handout by clicking this link.
EKG vs STEMI
Time to play everyone’s favorite game! Pericarditis vs STEMI. One goes home, the other goes to the Cath lab. No pressure, right?
It is critical to note that PR depression and Spodick’s Sign (downsloping of the TP segment in Lead II) are both not 100% reliable. Not even close. It is more reliable to rule out STEMI using the bullet points below and to proceed in descending order.
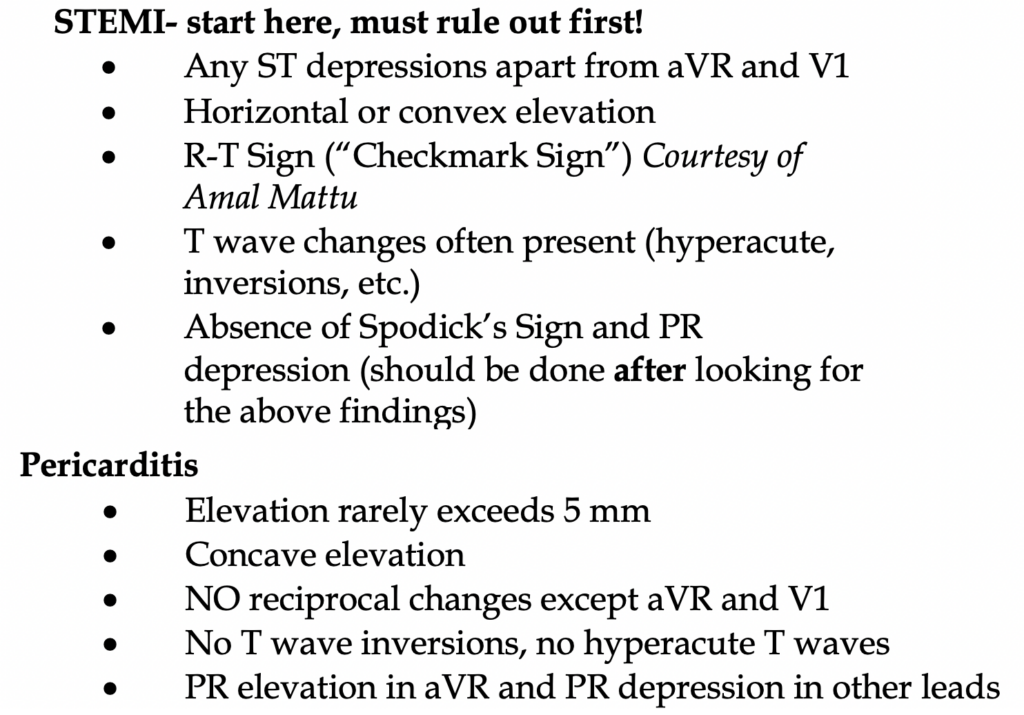
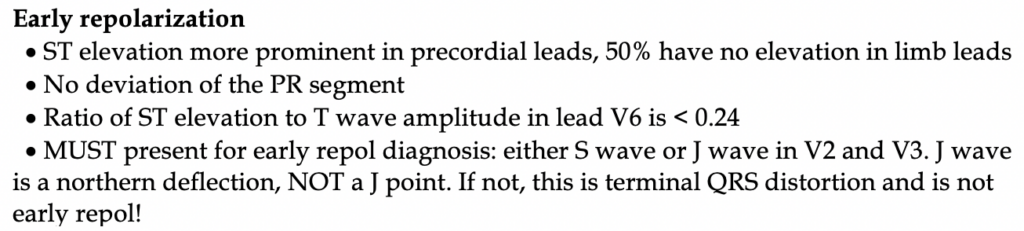
What about distinguishing pericarditis from early repolarization? Early repolarization is very common, nearly 30% in young adults. Both conditions have concave ST elevation, no inverted T waves, and no ST depression- ever.
Lab workup:
Labs are not helpful but rule out other causes. We would advise getting a troponin on these patients as the EKG is often unclear. If the troponin is elevated, this could be acute coronary syndrome or the patient has myopericarditis (~30% of patients with pericarditis have elevated troponins).8
Check a CBC, CMP, and CXR. We do not recommend CRP or ESR unless you are concerned about myocarditis. These are neither sensitive nor specific for pericarditis.
CXR is normal unless there is a large pericardial effusion. CXR should NOT be used to rule out effusion, as >200 mL is needed to even begin to show CXR changes.2
A bedside echo or formal study should be performed. In most cases of acute pericarditis, its normal. The presence of a pericardial effusion, however small, helps rule in pericarditis. Its absence, however, does not rule it out.
Diagnosis
>2 of the 4 strongly suggests acute pericarditis as a diagnosis:11
1. Sharp, pleuritic chest pain worse with sitting up
2. Auscultated friction rub
3. Consistent EKG changes
4. New or worsening pericardial effusion
Remember that although elevated levels of troponin are can be present in both pericarditis and myocarditis, they are not sensitive for either syndrome. When the troponin is elevated, higher levels are suggestive of myocarditis. Do not rely on other serologic markers including white cell count, ESR, and CRP as they have limited diagnostic value. 12
Causes
Rarely a cause is found.9 The majority of pericarditis cases are benign and idiopathic (>80%), with a likely viral etiology. Further definitive testing is not recommended.10 In one study, the causes that were found include neoplasia (5%), autoimmune diseases (5%), tuberculosis (4%). In patients who fail to improve, are hemodynamically unstable, have symptomatic effusions, or associated symptoms concerning for other pathologic processes, further testing should be sought.
Management
First, determine if the patient has pericarditis or myopericarditis. This might be difficult initially as they both present with nonspecific signs and symptoms with an ECG showing sinus rhythm or ST elevation. If there are features of myocarditis or myopericarditis, see our document on myocarditis. Key concerning echo findings are a low ejection fraction concerning for acute heart failure or significant pericardial effusion.
In those with a pericardial effusion who are symptomatic, a diagnostic and therapeutic pericardiocentesis can be performed by CT surgery or cardiology. This happens during admission. In the emergent setting where the patient is hemodynamically unstable, this is performed by you, the emergency physician. Effusions that are small to moderate with no associated hemodynamic dysfunction do not require drainage.13 If these patients are otherwise well with a small effusion, they can probably be discharged with good return precautions.
Disposition
There are no strict criteria for who should be admitted, but clearly, there is an element of “do the right thing” when it comes to thinking about who would benefit most from admission: any fever and/or elevated troponin (suggests developing myocarditis), >2 weeks of symptoms concerning for more insidious causes, evidence of moderate to large effusion, any tamponade pathology, any immunosuppressed or anticoagulated patients, failed outpatient course.4,8
Let’s sum that up: the decision to admit or discharge depends on 1) the presence of myocarditis, 2) the patient’s clinical status, and 3) echo findings.
Treatment
In those with idiopathic pericarditis who are being discharged, treatment is targeted at providing pain relief as well as reducing pericardial inflammation. In patients without contraindications, first-line therapy are NSAIDs +/- colchicine.14 There are lots of options, but we personally love ibuprofen 600 mg 3 times daily. Colchicine is dosed at 0.5 mg BID (See our gout document here on our breakdown of side effects of these therapies and contraindications). In those who have CAD, we avoid NSAIDs and prefer Aspirin 650 mg 3 times daily. Steroids should not be used initially but if there are contraindications NSAIDs, they may be used for 7-10 days. Restriction from strenuous physical activity is advised.15 If there is no response to therapy, this is concerning for an underlying cause, and admission with further testing is warranted.
References
1. Kytö V, Sipilä J, Rautava P. Clinical profile and influences on outcomes in patients hospitalized for acute pericarditis. Circulation 2014; 130:1601. 1
2. Chiabrando JG, Bonaventura A, Vecchié A, et al. Management of Acute and Recurrent Pericarditis: JACC State-of-the-Art Review. J Am Coll Cardiol 2020; 75:76. 2
3. Imazio M, Gaita F, LeWinter M. Evaluation and Treatment of Pericarditis: A Systematic Review. JAMA 2015; 314:1498. 4
4. Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol 2004; 43:1042. 5
5. Bösner S, Haasenritter J, Abu Hani M, et al. Accuracy of general practitioners’ assessment of chest pain patients for coronary heart disease in primary care: cross-sectional study with follow-up. Croat Med J. 2010;51(3):243-249. doi:10.3325//cmj.2010.51.243
6. Spodick DH. Pericardial rub. Prospective, Multiple observer investigation of pericardial friction in 100 patients. Am J Cardiol 1975; 35:357. 7
7. Zayas R, Anguita M, Torres F, et al. Incidence of specific etiology and role of methods for specific etiologic diagnosis of primary acute pericarditis. Am J Cardiol 1995; 75:378. 8
8. Imazio M, Demichelis B, Cecchi E, et al. Cardiac troponin I in acute pericarditis. J Am Coll Cardiol 2003; 42:2144. 20
9. Imazio M, Cecchi E, Demichelis B, et al. Indicators of poor prognosis of acute pericarditis. Circulation 2007; 115:2739. 6
10. Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation 2010; 121:916. 1*
11. Adler Y, Charron P, Imazio M, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC)Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J 2015; 36:2921. 28
12. Sharif N, Dehghani P. Emergency files: acute pericarditis, myocarditis, and worse!. Can Fam Physician. 2013;59(1):39-41.
13. Imazio M, Spodick DH, Brucato A, et al. Controversial issues in the management of pericardial diseases. Circulation 2010; 121:916. 23
14. Imazio M, Demichelis B, Parrini I, et al. Day-hospital treatment of acute pericarditis: a management program for outpatient therapy. J Am Coll Cardiol 2004; 43:1042. 8*
15. Pelliccia A, Solberg EE, Papadakis M, et al. Recommendations for participation in competitive and leisure time sport in athletes with cardiomyopathies, myocarditis, and pericarditis: position statement of the Sport Cardiology Section of the European Association of Preventive Cardiology (EAPC). Eur Heart J 2019; 40:19. 10*