Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Travis Smith, DO
Introduction
Myocarditis is inflammation of cardiac muscle caused by a variety of conditions. It has a variable presentation, ranging from acute to chronic inflammation, with focal to diffuse myocardial involvement. It has been recognized as a frequent cause of sudden cardiac death, up to 20% in young adults. It is commonly quoted that myocarditis is the most common cause of acute heart failure in patients <40 years old. Despite these frightening facts, it remains an elusive diagnosis, especially in children. This is likely because most cases are mild, resolve without sequelae, and those patients do not seek medical attention. In 2013, there were an estimated 22 per 100,000 cases worldwide. This review will cover the presentation, diagnosis, and management of myocarditis in adults.
Pathophysiology and Causes
Viruses are the most common pathogens, and over 20 viruses have been implicated as causes. Despite definitive testing, many viral causes remain unconfirmed (~50% of cases). There is no point in listing a table of viruses here, and the boards will not test on any particular ones except these: Coxsackie B virus, adenovirus, hepatitis C, cytomegalovirus, Epstein-Barr virus, HIV, and Parvovirus B19.
Other causes of myocarditis include bacteria, spirochetes, fungi, parasites (Trypanosoma cruzi), autoimmune (lupus), eosinophilic myocarditis, collagen vascular diseases, granulomatous diseases (sarcoidosis, giant-cell myocarditis), drugs/medications, toxins (cocaine), and even hypersensitivity reactions. The lists of many of these causative pathologies are long and not typically tested. We do not recommend memorizing specific causes.
In general, due to the vastness of potential causes of myocarditis, there is not a single, “red flag” that can be reliably remembered when collecting a history and suspecting myocarditis. We suggest focusing on the presentation and HPI more, as this will direct the workup.
Presentation
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Acute myocarditis is defined as a “condition with symptoms of heart failure over three months or less.” This is not very helpful to us in the ED as most patients present before clear evidence of heart failure is present.
There is high variability to the presentation, ranging from general fatigue to fulminant heart failure. There are no epidemiologic studies to help us define presenting symptoms.
Symptoms from systemic disease such as fever, headache, and myalgias can overshadow the more subtle cardiac signs, leaving it undiagnosed. There can also be a significant overlap with pericarditis, and some patients might present with symptoms such as retrosternal chest pain, or tachycardia out of proportion to their fever suggesting myopericarditis. See our handout on pericarditis for details.
Viral prodrome symptoms are reliably associated with only ~40% of cases.
“Tachycardia out of proportion to fever” is a good rule to use when approaching these patients.
Chest pain: usually a result of pericarditis. Myocarditis can mimic myocardial ischemia on EKG.
Heart failure: fatigue and decreased exercise tolerance are typically the earliest symptoms. There can be quick progression within days to weeks to right and left heart failure, manifesting in pulmonary congestion, JVD, reduced cardiac output, and peripheral edema.
Arrhythmias: sinus tachycardia is the most common, followed by various atrial arrhythmias.
There are no specific findings on the exam other than to look for signs of acute heart failure, such as a new murmur, fluid overload, JVD, and auscultating rales (suggestive of pulmonary edema).
Diagnosis
So, here’s the deal. We are stuck with a disease process that has no specific or sensitive markers to rule it out in the ED. What do you do? “Fire everything,” as they say on Star Trek.
It would be best if you throw a big net and hope you catch something. Inflammatory markers are what we are stuck with, along with your usual chest pain/fever workup.
EKG, troponin, BNP or BNP, CRP, ESR, CBC, CMP, chest x-ray are all useful.
EKG: there might be overlap with pericarditis findings. Look for signs of ischemia, much like you would for ACS. EKG is abnormal in up to 40% of cases with the most common arrhythmia encountered being sinus tachycardia, followed by various nonspecific rhythms (e.g., PACs, PVCs, A-fib, etc.).
If you can do a bedside echo, even better. Look for a qualitatively reduced ejection fraction, focal wall motion abnormalities, LV dilation, or pericardial effusion.
Although elevated in many other conditions, ESR and CRP have both been found to be elevated in 99% of patients with myocarditis.
Troponin is commonly elevated in patients with myocarditis as well.
A chest x-ray is not very helpful for identifying cardiomegaly but can demonstrate pulmonary edema or focal infiltrates concerning for pneumonia.
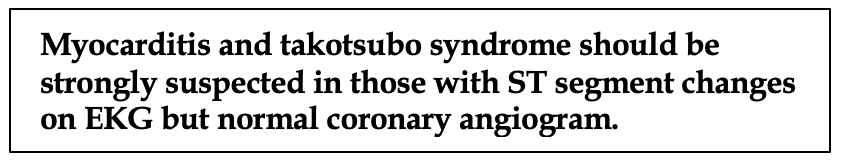
Coronary angiogram is indicated in those with STE consistent or suspicious for an MI, but if myocarditis is present, the patient will typically have a “clean cath”.
Endomyocardial biopsy is the most accurate test, but as you can imagine, it is not routinely performed and absolutely will not be available for ED physicians to use in their decision making.
So, when should you suspect this? The bottom line is myocarditis should be suspected in patients with or without cardiac signs who have the following: increased troponin, ischemic EKG changes, new arrhythmia, and evidence of reduced EF or focal wall abnormalities on echo. The diagnosis should be intensely suspected in those with a very low risk for ACS (e.g. young people and children), yet there are signs and symptoms of MI.
There are various, non-validated criteria that can be applied to attempt to definitely determine myocarditis as a cause during inpatient admission, but these are irrelevant to the ED physician. If there is a concern for myocarditis, the patient should be admitted – end of the story.
A robust differential diagnosis includes myocardial infarction, pericarditis (normal troponins), endocarditis, stress takotsubo cardiomyopathy.
Management
Admit all cases of suspected myocarditis.
If the patient is asymptomatic with EKG changes suggestive of ischemia, a good story, and elevated troponins but no evidence of heart failure = symptomatic management indicated; trend troponins. These patients have an excellent prognosis and a self-limited disease.
Patients with pericarditis symptoms and/or EKG findings, elevated troponins, but no evidence of heart failure = symptomatic management; trend troponins. These patients have myopericarditis and have low risk of heart failure, but need to be closely watched.
All patients with a new or worsening pericardial effusion should be admitted regardless.
Those with elevated troponins and evidence of acute heart failure have the potential to get really sick.
Fulminant myocarditis: any myocarditis with new onset heart failure requiring inotropic support either by parenteral drugs or mechanical support. They have a high mortality and complication risk (see below).
Standard therapy of acute heart therapy applies here: If in respiratory distress, NIPPV is indicated if patient qualifies. Endotracheal intubation is needed if NIPPV is contraindicated or patient fails NIPPV trial. Standard therapy of acute heart therapy applies here:
· IV Loop diuretic therapy
· Early initiation of ACEI therapy (rapid acting IV enalapril or captopril)
· Withhold beta blocker therapy in those with more than mild acute decompensated heart failure.
· Inotrope support in those with normal BP but depressed EF.
-Epinephrine monotherapy has been associated with an increase in 90-day mortality and worsening renal and cardiac markers.
-Dobutamine is preferred. In those on chronic beta-blocker therapy, a PDE-3 inhibitor (milrinone) is preferred as dobutamine is less effective.
-Warning: PDE-3 inhibitors are potent vasodilators. They cause afterload reduction, dilation of pulmonary vessels, and improved hemodynamics.
-Milrinone is more dysrhythmogenic than dobutamine. It also has a longer half-life.
· Norepinephrine +/- Inotropic support in those with hypotension is favored.
· Mechanical circulatory support (IABP) in those with refractory hypotension despite vasopressors and inotropic support.
-IABP increases systolic BP while offloading afterload and myocardial oxygen demand.
· Perform emergent pericardiocentesis at bedside if there is evidence of effusion in an unstable patient.
What about those with arrhythmias? Antiarrhythmic therapy should not be given in those with asymptomatic PAC or PVCs or non-sustained arrhythmias. If an antiarrhythmic must be given due to persistent, sustained rhythms, avoid Class I or III antiarrhythmics except for amiodarone (it’s really the only option here). If unstable with a tachydysrhythmia, immediate cardioversion should be performed while following standard ACLS protocols.
Antibiotics are rarely needed, unless in the setting of rheumatic fever, diphtheria, or meningococcemia.
Specific therapies: there are unique therapies that are indicated for certain causes of myocarditis, but this is not only beyond the scope of this handout but beyond the scope of the ED. Active discussion with cardiology and ICU should take place in these patients.
Prognosis
“Complicated myocarditis” includes any of the following EF <45-50%, sustained ventricular arrhythmias, poor cardiac output needing inotrope support or mechanical circulatory support. These patients have an average mortality rate of ~9%; mechanical circulatory support was needed in ~20%. This subset of patients went on to needing transplant (2%), cardiac death (2%), and sustained VT needing cardioversion (~4%).
In one study of patients with diffuse and focal myocarditis on imaging, complete LV recovery at six months occurred in 81%.
A significant number of patients might have lasting cardiomyopathy. One study showed out of 1230 patients, around 9% were found to have evidence of myocarditis.
References
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015; 386:743.
- Cooper LT Jr. Myocarditis. N Engl J Med 2009; 360:1526.
- Walsh TJ, Hutchins GM, Bulkley BH, Mendelsohn G. Fungal infections of the heart: analysis of 51 autopsy cases. Am J Cardiol 1980; 45:357.
- Bowles NE, Ni J, Kearney DL, et al. Detection of viruses in myocardial tissues by polymerase chain reaction. evidence of adenovirus as a common cause of myocarditis in children and adults. J Am Coll Cardiol 2003; 42:466.
- Drory Y, Turetz Y, Hiss Y, et al. Sudden unexpected death in persons less than 40 years of age. Am J Cardiol 1991; 68:1388.
- Caforio AL, Pankuweit S, Arbustini E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of myocarditis: a position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J 2013; 34:2636.
- Richardson P, McKenna W, Bristow M, et al. Report of the 1995 World Health Organization/International Society and Federation of Cardiology Task Force on the Definition and Classification of cardiomyopathies. Circulation 1996; 93:841.
- Dec GW Jr, Palacios IF, Fallon JT, et al. Active myocarditis in the spectrum of acute dilated cardiomyopathies. Clinical features, histologic correlates, and clinical outcome. N Engl J Med 1985; 312:885.
- Sarda L, Colin P, Boccara F, et al. Myocarditis in patients with clinical presentation of myocardial infarction and normal coronary angiograms. J Am Coll Cardiol 2001; 37:786.
- Blauwet LA, Cooper LT. Myocarditis. Prog Cardiovasc Dis 2010; 52:274.
- Aquaro GD, Perfetti M, Camastra G, et al. Cardiac MR With Late Gadolinium Enhancement in Acute Myocarditis With Preserved Systolic Function: ITAMY Study. J Am Coll Cardiol 2017; 70:1977.
- Howlett JG, McKelvie RS, Arnold JM, et al. Canadian Cardiovascular Society Consensus Conference guidelines on heart failure, update 2009: diagnosis and management of right-sided heart failure, myocarditis, device therapy and recent important clinical trials. Can J Cardiol 2009; 25:85.
- Howlett JG, McKelvie RS, Arnold JM, et al. Canadian Cardiovascular Society Consensus Conference guidelines on heart failure, update 2009: diagnosis and management of right-sided heart failure, myocarditis, device therapy and recent important clinical trials. Can J Cardiol 2009; 25:85.
- O’Connell, JB. Diagnosis and medical treatment of inflammatory cardiomyopathy. In: Cardiovascular Medicine, Topol, E, Nissen, J (Eds), Lippincott-Raven, Philadelphia 1998.
- Wentworth P, Jentz LA, Croal AE. Analysis of sudden unexpected death in southern Ontario, with emphasis on myocarditis. Can Med Assoc J 1979; 120:676.
- Imazio M, Brucato A, Barbieri A, et al. Good prognosis for pericarditis with and without myocardial involvement: results from a multicenter, prospective cohort study. Circulation 2013; 128:42.
- Ammirati E, Cipriani M, Moro C, et al. Clinical Presentation and Outcome in a Contemporary Cohort of Patients With Acute Myocarditis: Multicenter Lombardy Registry. Circulation 2018; 138:1088.
- Kühl U, Pauschinger M, Seeberg B, et al. Viral persistence in the myocardium is associated with progressive cardiac dysfunction. Circulation 2005; 112:1965.
- Rezkalla S, Kloner RA, Khatib G, Khatib R. Effect of delayed captopril therapy on left ventricular mass and myonecrosis during acute coxsackievirus murine myocarditis. Am Heart J 1990; 120:1377.
- Rockman HA, Adamson RM, Dembitsky WP, et al. Acute fulminant myocarditis: long-term follow-up after circulatory support with left ventricular assist device. Am Heart J 1991; 121:922.