Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Introduction
This guide serves a quick hit synopsis of IV glucocorticoid usage in the ED. Practitioners frequently abuse giving both PO and IV glucocorticoid as a nonspecific management option for many conditions. Glucocorticoids should be respected – and feared – for their potential to greatly disrupt human physiology. In general, practitioners overuse IV glucocorticoids even when oral dosing is shown to be equivocal. Here, we dispel a few myths and go through the top conditions that have evidence supporting clear benefit from IV glucocorticoid therapy in the ED.
Side effects of glucocorticoids
In the past, folks in the ED “ignored” the side effects of short-term glucocorticoid usage. We would say “I’m only giving one dose, or 5 days, or 10 days or therapy. Its less than one month, what could happen?” Possibly a lot. More and more data are coming out concerning glucocorticoid usage and their associated side effects. One population-based cohort study of >1.5 million Americans showed that within 30 days of a short-term prescription of oral glucocorticoid use, there were increase rates of sepsis, venous thromboembolism, and fracture within that 30-day period. Yes, there are plenty of confounding variables in this study, but it should raise awareness that glucocorticoids are not “angelic” therapies. Estimation regarding the frequency and severity of side effects and the highest risk dose associated with them are limited by small numbers of trials.
Glucocorticoids are associated a variety of cardiovascular effects, including fluid retention, hypertension, worsening atherosclerotic disease, certain arrhythmias, and even hyperlipidemia.
Glucocorticoids, not just NSAIDs, increase the risk of gastritis, ulcers, and upper-GI bleeding. NSAIDs and glucocorticoids together greatly increase the risk, a nearly 2-fold increased risk.
Glucocorticoids cause dose-dependent hyperglycemia, making glycemic control difficult for those with pre-existing diabetes mellitus.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Frequent usage of glucocorticoids
Infections
Let’s break the ice with the most controversial topic: glucocorticoids in septic shock.
As of this writing (late 2020), glucocorticoid therapy should be a case-by-case decision in select patients with refractory shock (SBP <90 mmHg for more than one hour following both adequate fluid resuscitation and vasopressor administration). This does NOT include patients who are glucocorticoid dependent or when adrenal insufficiency is suspected.
-Many RCTs and meta-analyses have shown glucocorticoids lead to faster resolution of shock; however, there appears to be minimal or no effect on mortality.
-If using steroids, only use hydrocortisone. Hydrocortisone 1 mg/kg delivered as a bolus or as an infusion was more likely than placebo and methylprednisolone to result in shock reversal.
Meningitis: controversial. Dexamethasone has been studied as an adjuvant therapy to reduce the neurological complications in adults and children. It is controversial and there’s a lot of chit-chat on this subject, but we’ll spare you and tell you what you need to know.
– In general, in developed countries, the guidelines recommend giving 0.15 mg/kg dexamethasone before or at the same time as antimicrobials if there is strong suspicion for bacterial meningitis, but the organism is unknown. It should only be continued if the organism is found to be S. pneumoniae. There is no proven benefit of continuing glucocorticoids if the organism is not S. pneumoniae.
– Dexamethasone should not be given after antibiotics as its benefit is very limited and there might even be an increase in mortality.
-In developing countries, dexamethasone has a less clear role and no proven benefit.
– In children, steroids are only indicated in those with H. influenzae B meningitis. It can reduce the risk of hearing loss. Glucocorticoids should be given prior to, or with the first dose of antibiotics and continued for 4 days. Since H. influenzae is exceedingly rare, we only give steroids in unvaccinated children with suspected meningitis.
– There has been a long-held concern that glucocorticoids may reduce antibiotic penetration into CSF (especially Vancomycin). This is controversial and will NOT be on boards.
Rheumatologic/autoimmune diseases
Multiple sclerosis exacerbation: well-established. IV methylprednisone reduces disability at 28 days. Oral prednisone has been studied and, in some cases, accepted, but we know from experience IV is preferred.
Temporal arteritis: well-established in preventing dreaded, irreversible vision loss. If visual symptoms or rapidly progressive disease symptoms are occurring, IV is absolutely indicated. If no visual symptoms are present, oral prednisone is perfectly acceptable.
Severe ITP: Glucocorticoid therapy is indicated when there is active bleeding and platelet counts of 10-20,000, or in those with no bleeding but platelet counts <10,000. Dexamethasone and prednisone raise the platelet count in approximately two-thirds of patients, with most patients responding within two to five days, thus decreasing the need for IVIG.
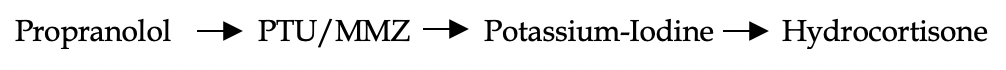
Thyrotoxicosis: IV glucocorticoids reduce T4-to-T3 conversion and possibly reduce the autoimmune process in Graves’ disease. They should not be given in hyperthyroidism absent of storm. They also should be given last. Here is the order you should give therapies:
Inflammatory bowel disease (IBD): if an exacerbation is suspected, consultation with a gastroenterologist is preferred prior to dosing. There are lots of reasons why a patient with IBD presents with a “flare”. Some causes are as simple as medication noncompliance and exacerbation of immunologic symptoms. Others are life-threatening such as toxic megacolon, abscesses, large fistulas, or small bowel obstruction. Obviously, steroids are not the solution in these cases. The clinician must exert utmost caution in having a large differential when these complicated patients present to the ED.
There is no data detailing the effectiveness of IV versus oral steroids in IBD. Methylprednisone is preferred and the patient can be transitioned to oral dosing once inpatient. Glucocorticoids are seen as short-term induction therapies or for exacerbations and should never be given long term.
Severe SLE flare: a “severe” flare is any patient with new renal insufficiency and significant proteinuria. This is suspected to be lupus nephritis which is the most common cause of death in SLE. Labs will show low C3, C4, and elevated acute phase reactants. IV methylprednisone is preferred. We suggest calling rheumatology first, as IV glucocorticoids may be very harmful if the diagnosis is not SLE, but scleroderma.
Respiratory illness
COPD/asthma exacerbations: IV glucocorticoids have been found to be equally efficacious as oral glucocorticoids. However, when a patient is in any sort of respiratory distress, we recommend IV as every effort should be made to optimize patient breathing. Don’t forget to give inhaled corticosteroids as well!
Glucocorticoids in COPD/asthma have a bevy of evidence behind them: decreased hospital stay, improved lung function and symptoms, reduced treatment failure risk by 50%, and even reduced relapse risk at 1 month.
Pneumocystis jiroveci pneumonia: glucocorticoids have been shown to decrease the mortality and risk of respiratory failure in those with severe Pneumocystis pneumonia. They should be given if:
– partial pressure of O2 <70 mmHg on room air and/or
– A-a gradient >35 on arterial blood gas
Even easier, if there is clear evidence of persistent hypoxemia (<92%) on pulse oximetry, don’t wait for the blood gas. Glucocorticoids can be given. Oral route is fine and works well, but given their respiratory distress, IV is preferable.
References
1. Short term use of oral corticosteroids and related harms among adults in the United States: population based cohort study. BMJ. 2017 Apr 12;357:j1415. doi: 10.1136/bmj.j1415.
2. Gabriel SE, Jaakkimainen L, Bombardier C. Risk for serious gastrointestinal complications related to use of nonsteroidal anti-inflammatory drugs. A meta-analysis. Ann Intern Med 1991; 115:787.
3. Olefsky JM, Kimmerling G. Effects of glucocorticoids on carbohydrate metabolism. Am J Med Sci 1976; 271:202.
4. American Academy of Pediatrics. Pneumococcal infections. In: Red Book: 2015 Report of the Committee on Infectious Diseases, 30th ed, Kimberlin DW, Brady MT, Jackson MA, Long SS (Eds), American Academy of Pediatrics, Elk Grove Village, IL 2015. P.626.
5. Annane D, Bellissant E, Bollaert PE, et al. Corticosteroids for treating sepsis. Cochrane Database Syst Rev 2015; :CD002243.
6. Annane D, Bellissant E, Bollaert PE, et al. Corticosteroids in the treatment of severe sepsis and septic shock in adults: a systematic review. JAMA 2009; 301:2362.
7. Brouwer MC, McIntyre P, Prasad K, van de Beek D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst Rev 2015; :CD004405.
8. Chaudhuri A. Adjunctive dexamethasone treatment in acute bacterial meningitis. Lancet Neurol 2004; 3:54.
9. de Gans J, van de Beek D, European Dexamethasone in Adulthood Bacterial Meningitis Study Investigators. Dexamethasone in adults with bacterial meningitis. N Engl J Med 2002; 347:1549.
10. Isenberg DA, Allen E, Farewell V, et al. An assessment of disease flare in patients with systemic lupus erythematosus: a comparison of BILAG 2004 and the flare version of SELENA. Ann Rheum Dis 2011; 70:54.
11. Minneci PC, Deans KJ, Eichacker PQ, Natanson C. The effects of steroids during sepsis depend on dose and severity of illness: an updated meta-analysis. Clin Microbiol Infect 2009; 15:308.
12. Minneci PC, Deans KJ, Natanson C. Corticosteroid therapy for severe sepsis and septic shock. JAMA 2009; 302:1643; author reply 1644.
13. Minneci PC, Deans KJ, Natanson C. Corticosteroid therapy for severe sepsis and septic shock. JAMA 2009; 302:1643; author reply 1644.
14. Mithoowani S, Gregory-Miller K, Goy J, et al. High-dose dexamethasone compared with prednisone for previously untreated primary immune thrombocytopenia: a systematic review and meta-analysis. Lancet Haematol 2016; 3:e489.
15. Mizutani H, Furubayashi T, Imai Y, et al. Mechanisms of corticosteroid action in immune thrombocytopenic purpura (ITP): experimental studies using ITP-prone mice, (NZW x BXSB) F1. Blood 1992; 79:942.
16. Sligl WI, Milner DA Jr, Sundar S, et al. Safety and efficacy of corticosteroids for the treatment of septic shock: A systematic review and meta-analysis. Clin Infect Dis 2009; 49:93.
17. Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 2004; 39:1267.