Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs
Objectives: define bowel obstructions and their types, pathophysiology, causes, presenting signs/symptoms, diagnosis, and treatment options, as well as the complications associated with them.
Bowel Obstruction: the prevention of the normal digestive process as well as intestinal motility. They make up 2-4% of emergency department visits annually in the US, and 15% of hospital admissions.
2 overarching categories:
Mechanical obstruction: More common. physical blockage of the GI tract. Can be complete or incomplete. Complete obstruction typically is more severe and more likely requires surgical intervention.
Functional obstruction: diffuse loss of intestinal motility and digestion throughout the intestine (e.g. failure of peristalsis).
2 possible locations:
Small bowel: more common (80% of cases).
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Large bowel
All bowel obstructions have the potential risk of progressing to complete obstruction
Mechanical obstruction
Pathophysiology
Mechanical blockage of flow —> dilation of bowel proximal to obstruction —> distal bowel is flattened/compressed —> Bacteria and swallowed air add to the proximal dilation —> loss of intestinal absorptive capacity and progressive loss of fluid across intestinal wall —> dehydration and increasing electrolyte abnormalities —> emesis with excessive loss of Na, K, H, and Cl —> further dilation leads to compression of blood supply —> intestinal segment ischemia and resultant necrosis.
Signs/Symptoms: The goal of the physical exam in this case is to rule out signs of peritonitis (e.g. ruptured bowel).
Colicky abdominal pain with abrupt onset (70-92%).
Bloating and distention: distention is worse in distal bowel obstruction. Hyperresonance on percussion.
Nausea and vomiting: 82%. Worse in proximal obstruction. Excessive emesis leads to hyponatremic, hypochloremic metabolic alkalosis with hypokalemia. Dehydration from emesis and fluid shifts results in dry mucus membranes and oliguria
Obstipation: severe constipation or complete lack of bowel movements (90%). Stool can still pass for 12-24 hr as the distal bowel compresses.
High pitched “tinkling noises” on auscultation: Unreliable in real life; it should never change management if you hear it/don’t hear it.
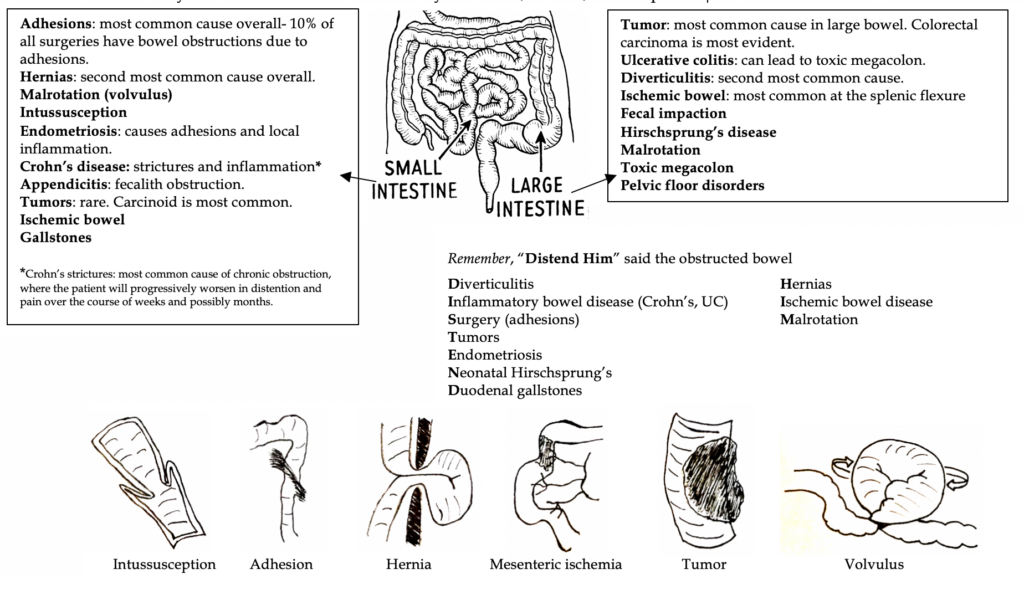
Causes: easiest to break them up in relation to small or large intestines, although there is definitely overlap and the two locations are not exclusive! Summary: 90% of obstructions are caused by adhesions, hernias, and neoplasms.
Diagnosis
Labs aren’t all that helpful. Possible leukocytosis which is nonspecific, and electrolyte abnormalities can occur as the obstruction progresses or via repeated emesis.
Anemia in this setting à think about a lower GI bleed due to colorectal carcinoma or Crohn’s.
Lactate —> modestly sensitive for infarction, lacks specificity. If elevated, be concerned for possible ischemia. On boards, if you encounter a bowel obstruction case and the lactate is elevated, assume ischemia is occurring.
Imaging: in hemodynamically unstable patients with evidence of peritonitis, an abdominal radiograph should be performed first: this determines if there are emergent issues and need for immediate surgery.
Typical findings that suggest SBO: dilated bowel loops and air fluid levels. dilation of bowel proximal to obstruction, distal is flattened/compressed
Free air under the diaphragm means hollow viscous injury! Antibiotics and immediate OR!
CT: in those who are clinically stable. Same results as above but in greater resonance. Do not use oral contrast. Besides dilated proximal bowel, distal collapsed bowel, and air fluid levels, other findings include: wall thickening, mesenteric edema and stranding, ascites.
Management
Therapy is broken up into 2 categories- conservative (nonsurgical) or surgical.
All patients need a surgical consult, but only a minority will actually need to go to the OR.
In general, if the patient is hemodynamically stable and has no other emergent comorbidities, conservative therapy is preferred until 1 or more of the following conditions occurs:
1) the patient deteriorates or fails to make any improvement after >48 hours (fever, tachycardia, worsening pain, leukocytosis, peritonitis) —> consider surgery.
2) there is evidence of bowel ischemia (lactic acidosis), necrosis, or perforation (free air on imaging)
3) the patient’s obstruction is secondary to a mechanical obstruction that requires surgical intervention (e.g. certain tumors, hernias, Hirschsprung’s, malrotation, appendicitis, Crohn’s strictures).
4) the patient’s condition resolves and no further intervention is necessary.
20-30% of patients will require operative intervention. Bowel ischemia, the scariest complication, occurs in 7-42% of cases.
Conservative therapy: the patient is dehydrated, electrolyte deficient, and distended due to accumulating air in the bowel. So, the treatment is based off managing that.
-make the patient NPO to prevent further distention and possible perforation.
-Nasogastric tube set to suction: reduces distention and risk for bowel perforation. This is critical and drastically reduces the need for surgery!
-IV fluids and electrolyte correction
-Manage the underlying cause. If inflammatory (Crohn’s or colitis), corticosteroids should be given, etc.
-Try to minimize from using opioids to treat pain as this further reduces gut motility.
-Antibiotics are warranted in those with C. difficile colitis, diverticulitis, or perforations.
Functional bowel obstruction
Postoperative Ileus: Most common cause of functional obstruction. It is due to normal physiologic factors that disrupt peristalsis. Usually lasts <24 hours in small bowel and <48 in large bowel. No intervention is warranted unless the patient suddenly becomes hemodynamically unstable. Typically, the patient does not have any pain if not mild discomfort.
Diagnosis: no mechanical obstruction or air fluid levels on imaging; only diffuse, dilated bowels.
Pathologic Ileus: An extension of the above condition. Marked by no stool >5 days after surgery, nausea/vomiting, and poor oral intake.
Causes: typically develops from postoperative ileus. Also, trauma, ischemia, and medications (opioids, anticholinergics).
Treatment: Ileus is managed conservatively.
Toxic Megacolon: acute, severe dilation of the colon that is due to massive inflammation à leads to a dilated and weak-walled colon due to destruction of the ganglionic cells in the muscularis propria. The risk to rupture is significant. These patients are seriously sick on presentation.
Causes are high yield: C. difficile, Chagas disease, Hirschsprung’s, Inflammatory bowel disease
Dx: massively dilated colon on plain film or CT with presentation consistent with above causes.
Tx: decompression. If failed, colectomy needed.