Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Authors: Payal Patel, MS4; Blake Briggs, MD
Introduction
Retropharyngeal abscess is a polymicrobial infection that most commonly occurs in children between the ages of two to four years (1). This is a sneaky infection that can become a major problem fast, as it involves a potential space that travels from the base of the skull to the posterior mediastinum. Per national databases, there was a significant increase in the incidence of retropharyngeal abscess from the years 2000 to 2012 (2). The most common bacterial species associated with retropharyngeal abscess include: Streptococcus pyogenes (GAS), Staphylococcus aureus (including MRSA), and respiratory anaerobes (Fusobacteria, Prevotella, and Veillonella species) (3). Half of all retropharyngeal abscess cases are associated with an antecedent upper respiratory tract infection (4). About a quarter of all retropharyngeal abscess cases (typically in older children or adults) are associated with pharyngeal trauma such as penetrating foreign body, endoscopy, intubation, and dental interventions (5). Let’s quickly review this classic HEENT pathology, its presentation, diagnosis, and management.
Anatomy
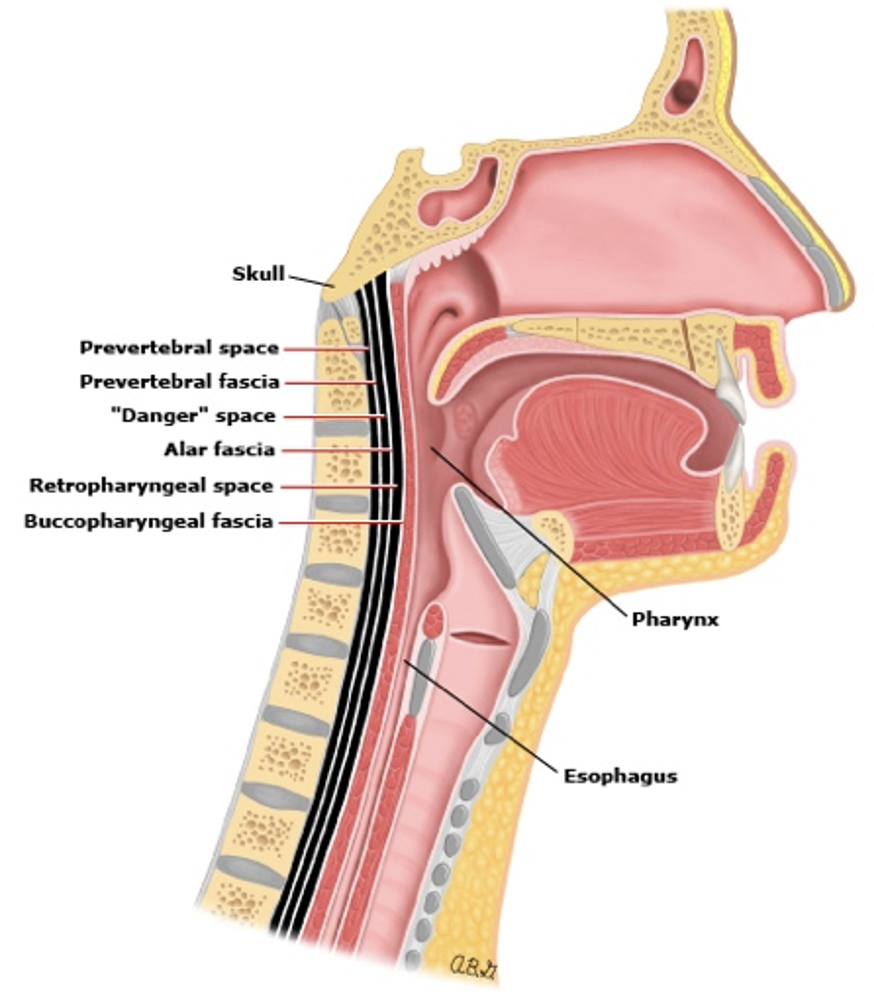
The retropharyngeal space is from the base of the skull to the posterior mediastinum, which communicates with the lateral pharyngeal space, as shown below (6). The lateral pharyngeal space is bounded by the carotid sheath, consisting of the carotid artery and jugular vein. The “danger zone” (cue Kenny Loggins and Maverick) is posterior to the retropharyngeal space and is a potential pathway for retropharyngeal infections to spread into the mediastinum (6).
Clinical Manifestations
What happens here is retropharyngeal nodes become infected and develop into cellulitis and possibly an abscess too.
These nodes are more pronounced in children and in fact you will almost always exclusively see these in children <6 years old (over 96% of them!).
The typical story and risk factor is a preceding head and neck infection (like otitis, pharyngitis, etc). Less commonly, a foreign body ingestion, or a child falling on a toothbrush in their mouth while running are examples of causes.
Early in the disease, findings are like that of uncomplicated pharyngitis.
Now in adults, a classic story is an accidentally swallowed foreign body causing an infection by puncturing the posterior pharynx, most specifically, a fish or chicken bone.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Children with retropharyngeal abscesses typically appear ill with moderate fever, dysphagia, odynophagia, drooling, decreased PO intake, neck stiffness, change in vocal quality, respiratory distress, neck swelling, and trismus.7 Chest pain is seen in patients with mediastinal extenstion (7).
The complications of RPAs are staggering: mediastinitis, airway obstruction, necrotizing infections, spread to the posterior column causing osteomyelitis or meningitis. Less commonly, jugular vein seeding, and thrombosis may occur. And those are just the highlights. There is a full table from most medical texts, but that would be boring to read.
A rule of thumb is to think about RPA in any child with fever, severe sore throat, and a normal pharyngeal exam.
Evaluation
Suspicion of retropharyngeal abscess warrants rapid assessment to determine extent of upper airway obstruction. Signs of airway obstruction include anxious appearing patients in the “sniffing position.”
Laboratory: like so many infections, labs alone are not sensitive or specific for RPAs.
Imaging: Includes lateral neck radiographs and/or CT neck with contrast.

If suspicion is low and no signs of airway compromise, the initial study is lateral neck radiograph (photo to the right) (8). It should always be obtained with extension on inspiration, because any other positioning method could result in false enlargement. There are these assigned numbers to how much enlargement of the prevertebral space should occur depending on the cervical vertebrae, but you don’t need to memorize these because they vary with age and the level of the cervical vertebrae. In general, it has been relegated to only those where you have a low suspicion for RPA, so that’s another reason to not do them.

If suspicion is high, CT with contrast is indicated (photo to the right). CT scans are test of choice, they can differentiate between retropharyngeal abscess and cellulitis and identify extension of abscess. If patient has respiratory distress, CT is omitted, and evaluation is in the OR. The red arrow in the photo points to the RPA.
Remember that both x-rays and CTs suffer some sensitivity and specificity issues, and therefore it is paramount that you have a high clinical suspicion first to guide your pre-test probability.
Management
Management includes similar items to epiglottitis. The most important piece is to maintain a position of comfort for the patient. Don’t force the child to lay on the bed. Instead, let the child sit in the mother’s lap if that’s best. Airway support is crucial here. Our premium podcast, EM Rapid Bombs, covers specific scenarios of how to approach these airways. Subscribe and you can check out the three-part series on this.
Patients that are toxic appearing (anxious, “sniffing position,” and marked suprasternal retractions) need a secure airway immediately. There’s no clear indication for surgical intervention in these patients, so you’ll never be tested on that, nor do you have to know about it.
In general, patients with retropharyngeal abscesses 2.5 cm2 and no airway compromise, antibiotic therapy trial for 24 to 48 hours should be initiated without surgical drainage (9).
Antimicrobial therapy:
Empiric treatment covering for GAS, S. aureus, and respiratory anaerobes:
- Ampicillin-sulbactam + Clindamycin
Failed response to empiric treatment or moderate/severe disease:
- Ampicillin-sulbactam OR Clindamycin + Vancomycin OR Linezolid
Oral therapy 14 days after patient is afebrile and clinically improved:
- Amoxicillin-clavulanate OR Clindamycin (10)
All these patients are ICU admissions, every time. That’s easy enough.
References
1. Craig FW, Schunk JE. Retropharyngeal abscess in children: clinical presentation, utility of imaging, and current management. Pediatrics. 2003 Jun;111(6 Pt 1):1394-8. doi: 10.1542/peds.111.6.1394. PMID: 12777558.
2. Woods CR, Cash ED, Smith AM, Smith MJ, Myers JA, Espinosa CM, Chandran SK. Retropharyngeal and Parapharyngeal Abscesses Among Children and Adolescents in the United States: Epidemiology and Management Trends, 2003-2012. J Pediatric Infect Dis Soc. 2016 Sep;5(3):259-68. doi: 10.1093/jpids/piv010. Epub 2015 Mar 22. PMID: 26407249.
3. Asmar BI. Bacteriology of retropharyngeal abscess in children. Pediatr Infect Dis J. 1990 Aug;9(8):595-7. PMID: 2235179.
4. Philpott CM, Selvadurai D, Banerjee AR. Paediatric retropharyngeal abscess. J Laryngol Otol. 2004 Dec;118(12):919-26. doi: 10.1258/0022215042790538. PMID: 15667676.
5. Sethi DS, Chew CT. Retropharyngeal abscess–the foreign body connection. Ann Acad Med Singap. 1991 Sep;20(5):581-8. PMID: 1781639.
6. Tebruegge M, Curtis N. Infections related to the upper and middle airways. In: Principles and Practice of Pediatric Infectious Diseases, 5th ed, Long SS, Prober CG, Fischer M (Eds), Elsevier Saunders, New York 2018. p.208.
7. Page NC, Bauer EM, Lieu JE. Clinical features and treatment of retropharyngeal abscess in children. Otolaryngol Head Neck Surg. 2008 Mar;138(3):300-6. doi: 10.1016/j.otohns.2007.11.033. PMID: 18312875.
8. Goldstein NA, Hammersclag MR. Peritonsillar, retropharyngeal, and parapharyngeal abscesses. In: Textbook of Pediatric Infectious Diseases, 8th ed, Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ (Eds), Saunders, Philadelphia 2019. p.119.
9. McClay JE, Murray AD, Booth T. Intravenous antibiotic therapy for deep neck abscesses defined by computed tomography. Arch Otolaryngol Head Neck Surg. 2003 Nov;129(11):1207-12. doi: 10.1001/archotol.129.11.1207. PMID: 14623752.
10. Tebruegge M, Curtis N. Infections related to the upper and middle airways. In: Principles and Practice of Pediatric Infectious Diseases, 5th ed, Long SS, Prober CG, Fischer M (Eds), Elsevier Saunders, New York 2018. p.208.