Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Editor: Salar Rafieetary, MD
Introduction 1-3
On this topic, we invited Salar Rafieetary, an ophthalmologist from Memphis, TN, to discuss some key points of management. He’s seen more hyphemas than he cares to discuss. You can read more about him at the end of this document.
Hyphema is defined as a collection of blood in the anterior chamber of the eye. Most commonly, hyphema is commonly seen in the setting of blunt or penetrating ocular trauma. Spontaneous hyphema, although less common, can be seen in the setting of blood dyscrasias (leukemia, lymphoma), vascular diseases (proliferative diabetic retinopathy, retinal vein occlusion), intraocular neoplasms (retinoblastoma, juvenile xanthogranuloma), and others. The most feared complication of hyphema is elevated intraocular pressure, which if undetected and/or untreated, can result in irreversible vision loss. Hyphemas make up 12 per 100,000 population, with males being 5 times as affected as females. Ocular protection would likely significantly decrease the rate of hyphemas.
In children, sports injuries are the most common cause. In teenagers and young adults, think assault or paintball/airsoft guns.
Also, think airbag deployment in motor vehicle crashes, or occupational exposure.
Brief anatomy
The anterior chamber is made up of the cornea, iris, angle, and lens. Clear aqueous humor fills that space. Aqueous humor is produced by the ciliary body and drains into the trabecular meshwork, near the junction of the iris and cornea. In the setting of hyphema, both red blood cells (RBCs) and macrophages engulfed with RBC breakdown products can obstruct the trabecular meshwork, resulting in elevated intraocular pressure (IOP). Elevated intraocular pressure, if untreated, can lead to irreversible vision loss.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Presentation
Trauma is the most common cause of hyphema. Blunt trauma (such as airbag or fist) is more common than penetrating.
Obviously, penetrating trauma presents a much higher risk of globe rupture.
A hyphema appears as a layering of blood in the anterior chamber. This can often be visualized by a clinician with the naked eye. However, the absence of a layered hyphema on gross inspection does not rule out the presence of hyphema. If the suspicion is high based on the mechanism of injury, Ophthalmology should be consulted for evaluation with a slit lamp.
Most patients present with photophobia and decreased visual acuity. Anisocoria may occur when there are torn iris sphincter muscles. Iridodialysis (iris tears away from its insertion) can also occur. An abnormal shape of the pupil should raise clinical suspicion of a potential globe rupture. Elevated IOP can be found in 30% of hyphema patients. 4,5
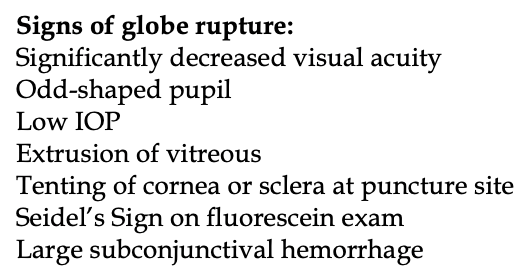
Physical exam should be thorough, and its main goal is to exclude an open globe. No tonometry, orbital ultrasound, or eyelid retraction should occur until an open globe has been excluded. This should be performed by an ophthalmologist.
Concerning signs of globe rupture are pictured to the right.
CT head should be performed if there is any suspicion for an open globe.
Always have a standard order when performing the eye evaluation: gross eye assessment —> visual acuity —> assess for pupillary light reflex and the presence of an afferent pupillary defect —> check intraocular pressure (if no signs of globe rupture) —> extraocular eye movements —> visual fields by confrontation.
Checking intraocular pressure is a very critical step when assessing patients with hyphema. Apply 1 drop of topical anesthetic (i.e. proparacaine or tetracaine). Tono-Pen® and iCare® are usually available in the ED setting. Gently lift the upper lid with careful attention not to press on the globe, which give an artificially elevated IOP. This step can be challenging in instances when there is significant periorbital swelling.
Fluorescein staining and examination with a blue light can be performed if the patient is complaining of foreign body sensation or the mechanism of injury (i.e., shattered windshield) increases clinical suspicion for a concurrent corneal abrasion.
In all cases of ocular trauma, fundus examination with a direct ophthalmoscope should be attempted to assess for vitreous hemorrhage, retinal detachment or commotio retina.
There is a grading system measured in height from inferior limbus to the top: 2
Grade I = 33%
Grade II = <50%
Grade III >50%
Grade IV = 100%
Risk of vision loss depends on degree and duration of elevated IOP and any rebleeding episodes.
We’ll be honest, we don’t memorize the grading system. Any hyphema regardless of size should be seen by an Ophthalmologist or at least followed outpatient daily.
Sickle cell disease (SCD) presents its own issues: those with sickle cell or trait have a higher risk of increased IOP, optic atrophy, and secondary hemorrhage. Sickling is more likely in low O2 environment (i.e. aqueous humor). 3,4 Given the high risk for complications and the high prevalence of sickle trait, a screening hemoglobin electrophoresis should be ordered of any African American or Hispanic patient, and anyone else with a positive family history for sickle cell or sickle trait.
Coagulopathies and other bleeding diatheses present a high risk of “spontaneous hyphema”. Diabetes mellitus, ocular cancers, and blood thinners increase the risk of this occurring. 4
Steps of management summarized: 6-8
- Elevate head of bed
- Apply rigid eye shield. Patient should wear this at all times.
- Correct coagulopathy if present- this is considered a life-threatening bleed that likely needs reversal. You should coordinate this with ophthalmology.
- Order a hemoglobin analysis for those with a family history of SCDIf positive, discuss with Ophthalmology. These patients are at high risk for losing vision!
- Those with known blood dyscrasias or coagulopathies need CBC, PT/INR/PTT testing.
Specific treatment for elevated IOP (>22 mmHg): 6-8
- Cycloplegics only if open globe is excluded
- Topical timolol is first line for elevated IOP management
- Avoid carbonic anhydrase inhibitors (CAIs) in those with SCD. This includes systemic acetazolamide and topical dorzolamide or brinzolamide.
- Avoid NSAIDs in those at higher risk of bleeding and SCD patients.
Open globe management: apply eye shield, IV antibiotics, emergent ophthalmology consult, aggressive antiemetics, and pain control.
Disposition
Hospital admission and emergent ophthalmology consult in the ED is required for the following:
– Every hyphema Grade III and IV
– Any patient with a coagulopathy, sickle cell hemoglobinopathy, or sickle cell trait
– Severely elevated IOP
– Those presenting with rebleeding hours to days later
Otherwise, if visual acuity is reassuring, pain under control, and open globe has been excluded, 24-hour follow up with ophthalmology is appropriate. An eye shield should be applied. There should be good communication and transition of care with Ophthalmology. These patients should be closely followed especially during days 3-7, as this is the when the risk of rebleeding is highest.
Ophthalmology may want to prescribe glucocorticoid drops in addition to cycloplegic eye drops.
Instruct patients to limit activity for one week. This means bedrest with bathroom privileges only. Encourage them to wear the shield at all times and avoid bending, squatting or lifting any objects over 10 lbs. These things can all increase risk of rebleed. They should return to the ED should any change in visual acuity or pain occurs, as secondary hemorrhage is a real concern and major complication.
Dr. Salar Rafieetary is a PGY-4 ophthalmology resident at Hamilton Eye Institute in Memphis, TN. He completed his medical school at UTHSC, graduating as an AOA member, GHHS member, as well as class president all four years. A native of the city, Dr. Rafieetary is passionate about the care his patients receive and will be completing his retina fellowship at Charles Retina Institute as well.
References:
1. Kennedy RH, Brubaker RF. Traumatic hyphema in a defined population. Am J Ophthalmol 1988; 106:123.
2. Edwards WC, Layden WE. Traumatic hyphema. A report of 184 consecutive cases. Am J Ophthalmol 1973; 75:110.
3. Walton W, Von Hagen S, Grigorian R, Zarbin M. Management of traumatic hyphema. Surv Ophthalmol 2002; 47:297.
4. Brandt MT, Haug RH. Traumatic hyphema: a comprehensive review. J Oral Maxillofac Surg 2001; 59:1462.
5. Sankar PS, Chen TC, Grosskreutz CL, Pasquale LR. Traumatic hyphema. Int Ophthalmol Clin 2002; 42:57.
6. Sankar PS, Chen TC, Grosskreutz CL, Pasquale LR. Traumatic hyphema. Int Ophthalmol Clin 2002; 42:57.
7. Brandt MT, Haug RH. Traumatic hyphema: a comprehensive review. J Oral Maxillofac Surg 2001; 59:1462.
8. Walton W, Von Hagen S, Grigorian R, Zarbin M. Management of traumatic hyphema. Surv Ophthalmol 2002; 47:297.