Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Christopher Musselwhite, MD
Peer Reviewer: Blake Briggs, MD
Objectives: Discuss the presentation, anatomy, and management of epistaxis.
Introduction
Epistaxis is a common complaint that affects approximately 60% of people in the US, with one study showing one-third of all households having one member of the household with recurrent, minor nosebleeds. It occurs more frequently in the young and the old, with only a few (<10% of total cases) trickling their way into the ED for help.1 Most nosebleeds are self-limiting, requiring minimal interventions to control, but some nosebleeds are reminiscent of “The Shining” elevator scene. This review will provide insight into some brief anatomy and physiology of nosebleeds, focusing on their management and disposition.
Pathophysiology
Nosebleeds are classified by their anatomic location, either anterior or posterior. The most common nosebleeds are anterior (up to 90%), occurring at Kiesselbach’s plexus (which is really fun to say; go ahead, say it a few times).2 The Kiesselbach’s plexus occurs at the confluence of several arterial branches you do not need to know. Anterior bleeds are typically minor and can be controlled with direct pressure or packing techniques as described below.
Posterior bleeds, on the other hand, are derived from larger, higher pressure arteries and can subsequently induce life threatening levels of bleeding. The most common source are branches of the sphenopalatine artery, originating off the external carotid artery system. Rarely, direct branches can come off the carotid system as well.
Causes and Risk Factors
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
There are many risk factors that predispose to higher rates of nosebleeds, or those which are resistant to standard therapies in the ED. Common causes are processes that affect the mucosa, such as dryness (as with central heat in the winter, or chronic oxygen use via nasal cannula). Anything that makes the mucosa friable is another risk, as with viral or bacterial infections, digital trauma via nose picking, or vasoactive substances like cocaine. Prior radiation therapy to the face can damage blood vessels and tissue, making them more likely to rupture. Other, less common causes can include active or prior local neoplasm or hereditary hemorrhagic telangiectasia (Oscar-Weber-Rendu). The latter is often diagnosed when patients present with repeated, difficult to control epistaxis episodes from arterial-venous malformations within the mucosa.3
One of the most common risk factors is anticoagulation and antiplatelet medications, followed by bleeding disorders. Remember, if asked on the test, the most common inherited bleeding disorder is vWF disease.
Patients rarely require reversal from their anticoagulation. In fact, in those who are hemodynamically stable, with an appropriate INR level (normal or therapeutic if on warfarin), then it is not recommended to reverse them.4
In children, nose picking is the most common cause. If there is purulent drainage present with epistaxis, consider the presence of a foreign body.
Assessment and Management
The algorithm below provides a nice overview of the typical management of epistaxis. The assessment and management of epistaxis is more of an art, as there are multiple valid approaches. However, one key will be to identify the stable versus unstable patient, taking appropriate resuscitation steps. The identification of posterior bleeds is also important, although somewhat difficult. Often, patients simply present with a nosebleed of unknown origin, and the management will be very similar for everyone, at least initially. However, posterior epistaxis will continue to bleed despite initial measures, which should create suspicion for a posterior source and additional appropriate actions.
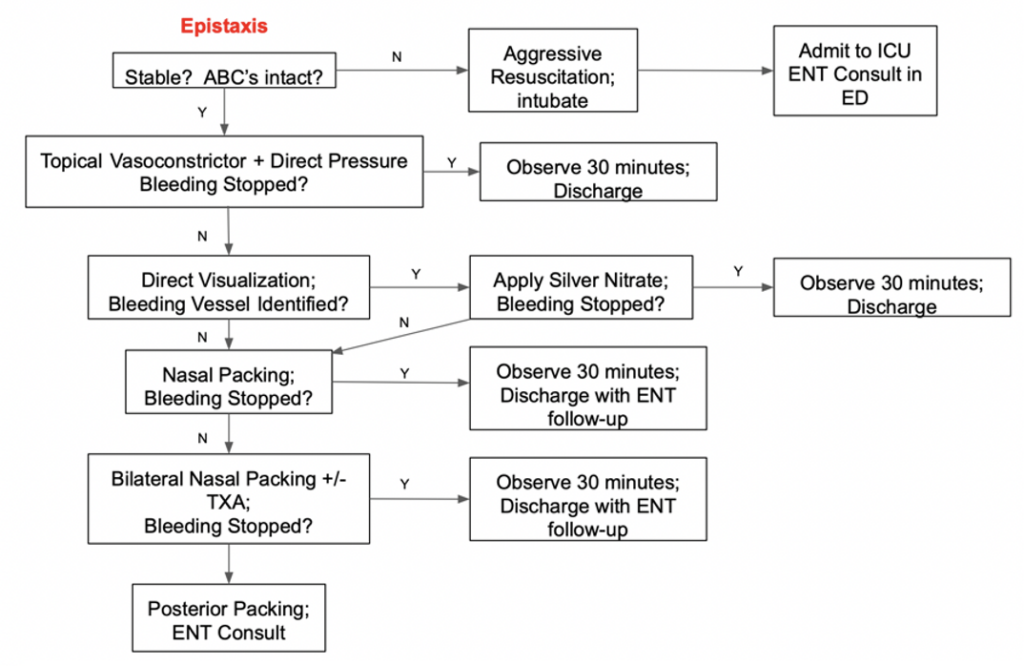
As aforementioned, airway, breathing, circulation should always be the first step in evaluation and management. If the patient has appropriate mental status, respirations, and vital signs, only then can you attend to the complaint of epistaxis. Posterior bleeds may be so significant that the patient may require an airway, or even emergent transfusion, making two large bore intravenous lines a must. Consider giving the patient a basin to spit blood in for patient comfort, as spitting the blood will prevent ingestion and the resultant nausea and vomiting associated with ingestion of blood.
Your first measure: topical vasoconstrictor sprays, like oxymetazoline, combined with direct pressure. A vasoconstrictor works best if the patient first blows their nose to expel any old clots prior to drug application. This often-forgotten step exposes the vasculature and fresh mucosa. Another key is to have the patient lean forward rather than leaning back, letting the blood flow out the nose rather than down the throat. Direct pressure is best applied via pinching the nasal alae together for at least 5-10 minutes. Time should always be taken to explain this method to patients and family at bedside. If bleeding ceases, the patient can be observed for 30 minutes for rebleeding and if no bleeding recurs, we discharge home with a topical antibiotic ointment (helps with lubrication) and do not pack the nose.

If the bleeding persists after direct pressure, consider attempting direct visual examination of the nares, hopefully being able to visualize the culprit vessel if it is anterior. This is best achieved using a nasal speculum (photo to the right), with one blade oriented superiorly and the other inferiorly (photo to the right demonstrates proper technique). Otoscopes are not as good.5
The vessel can then be cauterized with chemical cautery (silver nitrate). Never apply for >10 seconds. Silver nitrate should not be used bilaterally, because of the risk of septal perforation. It also only works on a minimally bloody surface. Any active bleeding will render it useless. Electrical cautery should be saved only for the otolaryngologist.

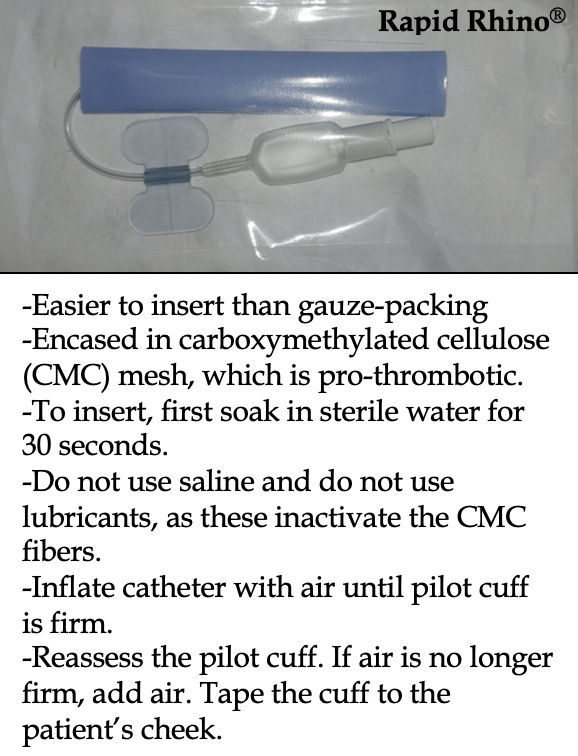
If the bleeding persists after cautery, or you are unable to visualize the bleeding vessel, it’s time for nasal packing. It is difficult to distinguish anterior from posterior nasal bleeding. Neither the briskness nor amount of bleeding will help. Insert packing deep to ensure potential any deeper sources of bleeding are identified. Anxiolytics prior to packing would be considerate, as the process is quite uncomfortable (if you have ever been swabbed for COVID-19, you have an idea of how bad it can be). Remember this is inflamed, friable, bleeding tissue, so it is swollen and painful. Achieve anesthesia with cotton swabs soaked in lidocaine with epinephrine. Several different commercial products for anterior packing are available, some designed to expand when wet, others that require inflation of a balloon. To the right below is a picture of the Rapid Rhino®, one commonly used and talked about. Another commonly used item is Merocel® tampons, which are inserted than flushed with TXA or water to rapidly expand. If you do not have these supplies, you can use ribbon gauze packed accordion-style into the nares.
TXA has very limited evidence but has been adopted in the ED for refractory cases. One approach is to use a Merocel® tampon soaked with 500 mg of the IV formulation of TXA. One meta-analysis of three RCTs with 408 patients found no statistical difference in short-term bleeding cessation but reported less rebleeding and greater patient satisfaction when TXA was used.6 We do not routinely use TXA due to its price at our shop, but it can be a worthy agent in refractory cases when you are packing the nose.
Nasal packing for anterior bleeding is 90-95% successful. In fact, if bleeding continues after packing, then consider bilateral packing. If bilateral packing does not stop the bleeding, then this is a posterior bleed until proven otherwise. Besides using longer length balloon catheters, there is not much more in the ED we can definitively do for posterior bleeds, so this should trigger an otolaryngology consult as well as admission to monitor the bleed with possible future procedures. If you are in a rural shop and alone, you can attempt using a 10 to 14 Fr Foley catheter, inserting through the nose along the pharynx until it is visible in the posterior oropharynx. Inflate then retract up against the posterior nasopharynx. Anterior nosebleeds rarely require admission, and that decision depends on the patient’s medical comorbidities as well as their ability to follow-up if they are high risk.
But what about the labs?
You’re probably asking about the CBC and coagulation studies. Well, we don’t get them unless the patient is unstable and/or being admitted. If you plan to send the patient home, don’t bother wasting your time as they rarely if ever change management.7
Are antibiotics needed upon discharge?
Systemic antibiotics are sometimes still given as prophylaxis against infectious complications from nasal packing. However, the evidence is poor that systemic antibiotics provide any benefit, especially if the packing is removed after 24 to 48 hours, and the patient is not immunocompromised. The decision to use prophylactic antibiotics should be made on a case-by-case basis, hopefully with input from your local otolaryngologist. Packing should never remain in place for >48 hours.
References
1. Petruson B, Rudin R. The frequency of epistaxis in a male population sample. Rhinology 1975; 13:129.
2. Alvi A, Joyner-Triplett N. Acute epistaxis. How to spot the source and stop the flow. Postgrad Med 1996; 99:83.
3. Shah RK, Dhingra JK, Shapshay SM. Hereditary hemorrhagic telangiectasia: a review of 76 cases. Laryngoscope 2002; 112:767.
4. Nitu IC, Perry DJ, Lee CA. Clinical experience with the use of clotting factor concentrates in oral anticoagulation reversal. Clin Lab Haematol 1998; 20:363.
5. Riviello RJ. Otolaryngologic procedures. In: Clinical Procedures in Emergency Medicine, 4th, Roberts JR, Hedges JR (Eds), WB Saunders, Philadelphia 2004. P.1300.
6. Gottlieb M, DeMott JM, Peksa GD. Topical Tranexamic Acid for the Treatment of Acute Epistaxis: A Systematic Review and Meta-analysis. Ann Pharmacother 2019; 53:652.
7. Thaha MA, Nilssen EL, Holland S, et al. Routine coagulation screening in the management of emergency admission for epistaxis–is it necessary? J Laryngol Otol 2000; 114:38.
8. Badran K, Malik TH, Belloso A, Timms MS. Randomized controlled trial comparing Merocel and RapidRhino packing in the management of anterior epistaxis. Clin Otolaryngol 2005; 30:333.
9. Singer AJ, Blanda M, Cronin K, et al. Comparison of nasal tampons for the treatment of epistaxis in the emergency department: a randomized controlled trial. Ann Emerg Med 2005; 45:134.