Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD, Shad Baab, MD
Introduction
Pediatric Sepsis is a significant cause of non-traumatic child mortality in the US. Like adults, early recognition and treatment can reduce morbidity and mortality by 50%.1 One of the key differences between adults and pediatric SIRS criteria is that one of the values needed must be fever or hypothermia. The others are straightforward:
– Fever or hypothermia (>38.5 or <36 C). Must be present!
– Tachycardia
– Tachypnea
– Leukocytosis or leukopenia
– Bandemia (>10%)
Presentation
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
How do you separate a child who simply needs ibuprofen/acetaminophen and rechecked vitals in the ED versus another child who needs IV fluids, antibiotics, and admission?
Well, it’s not easy, but this is where having experience really helps.
There is no single pathognomonic finding that defines shock.
Tachycardia is really the only way to increase cardiac output in children – so don’t wait for hypotension to start treating aggressively.
Things that should stick out to you on exam: poor perfusion, poor pulse quality, altered mental status.
More subtly, children who have not been feeding well appear irritable or lethargic.
What about “cold shock” findings? Cold shock is more common in children compared to adults.
– Expect cold, clammy extremities
– Less commonly extremities will be mottled or even cyanotic
– Capillary refill >2 seconds (in particular, centrally on the chest wall
– Thready pulses
Altered mental status and poor peripheral pulse quality are the two findings most associated with development of organ dysfunction.2
Diagnosis
Like adults, a broad look for infectious source is required.
Fingerstick glucose (hypoglycemia is not rare in septic children!), CBC, blood culture, lactate, chemistry panel, urinalysis and culture, inflammatory biomarkers.
Ionized calcium levels are needed because hypocalcemia is a risk in septic children.
Chest x-ray should be performed as well.
Management
Children do not have large reserves. Those who are fluid-refractory or catecholamine-resistant might need intubation to assist with ventilation and oxygenation.
Intubation reduces work of breathing, cardiac output, and improves perfusion to other organs. Remember that ketamine is the preferred induction agent.
Be aggressive! You will start with broad spectrum antibiotics. Not able to get an IV? IO is your friend here. Central lines are good to have, but never let their placement delay care!
Broad spectrum antibiotics: give within one hour of presentation if in shock, otherwise, give within 3 hours.
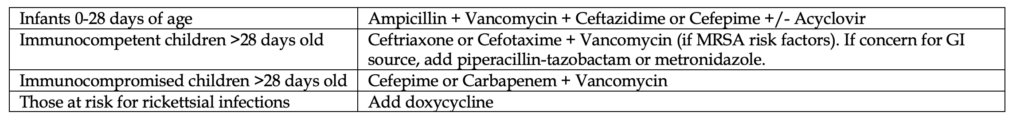
Antibiotic selection is in the table below. This selection depends on age and immune status. See our handout on Neonatal Fever for details on those patients.
There’s been some debate on the optimal IV fluid amount in children. Right now, 40-60 mL/kg pushed rapidly is a great place to start. Stick with isotonic fluids. Within the first hour, you need to determine if the patient is responding to fluids or not. In younger patients watch for worsening condition due to fluid overload from undiagnosed congenital heart disease.
While the fluids are flowing in, consider other causes of shock in children.
– Do a bedside ultrasound to look for a pericardial effusion/tamponade, overall cardiac function, and “squeeze”
– Do a chest x-ray and ultrasound to look for pneumothorax
– Use bedside ultrasound to see if there is free fluid in the abdomen
The key theme here is using bedside ultrasound, so make sure you practice. Typically, anatomic windows are easier to achieve in children with ultrasound compared to adults.
The decision to initiate vasopressors should come quickly. After you push the fluid bolus, if there is minimal change in their status, start them.
Children that are fluid-refractory respond well to vasopressors (epinephrine or norepinephrine).3
Like adults, there is no data to support that peripherally infused vasopressors are harmful, and if you do not have central access, never wait to start vasopressors. Two studies have shown that peripheral vasopressors are safe.4,5
There has been debate in the past on the choice of vasopressor, but recent literature suggests more and more that epinephrine is the right answer over dopamine.
Two small, randomized trials showed the following4,5:
– Epinephrine resolved refractory shock faster than dopamine.
– Survival rate was higher in those who received epinephrine.
Epinephrine: start with 0.05 to 0.1 mcg/kg/minute (rapidly titrate up to 1 mcg/kg/min and then add second vasopressor as needed)
Norepinephrine: start with 0.05 to 0.1 mcg/kg/minute (rapidly titrate up to 1 mcg/kg/min and then add second vasopressor as needed)
What about those with resistant septic shock? So, you’ve tried vasopressors and if still no response, stress dose hydrocortisone is the way to go (2-4 mg/kg/day).
References
1. Han YY1, Carcillo JA, Dragotta MA, Bills DM, Watson RS, Westerman ME, Orr RA. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003 Oct;112(4):793-9. PMID: 14523168.
2. Scott HF1, Donoghue AJ, Gaieski DF, Marchese RF, Mistry RD. Effectiveness of physical exam signs for early detection of critical illness in pediatric systemic inflammatory response syndrome. BMC Emerg Med. 2014 Nov 19;14:24. PMID: 25407007.
3. Ceneviva G1, Paschall JA, Maffei F, Carcillo JA. Hemodynamic support in fluid-refractory pediatric septic shock.Pediatrics. 1998 Aug;102(2):e19. PMID: 9685464.
4. Ramaswamy KN1, Singhi S, Jayashree M, Bansal A, Nallasamy K. Double-Blind Randomized Clinical Trial Comparing Dopamine and Epinephrine in Pediatric Fluid-Refractory Hypotensive Septic Shock. Pediatr Crit Care Med. 2016 Sep 23. PMID: 27673385.
5. Ventura AM1, Shieh HH, Bousso A, Góes PF, de Cássia F O Fernandes I, de Souza DC, Paulo RL, Chagas F, Gilio AE. Double-Blind Prospective Randomized Controlled Trial of Dopamine Versus Epinephrine as First-Line Vasoactive Drugs in Pediatric Septic Shock. Crit Care Med. 2015 Nov;43(11):2292-302. PMID: 26323041.