Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Larry Mellick, MD, Ron Waldrop, MD
Introduction (1-3)
Febrile seizures are the most common neurologic disorder in children. They are age-dependent and occur in 2-4% of children between 6 months and 5 years old, with a peak incidence at 15 months. It is an event associated with fever but no evidence of intracranial infection or defined cause. It is not a form of epilepsy. This review will cover definitions of febrile seizures, classifications, and management.
Pathophysiology and risk factors (4-5)
Their exact mechanism is unclear, but likely is related to the vulnerability of the nervous system when the body has a fever. There likely is a genetic connection as well.
The rate of rise of a fever is not a risk factor, while the maximum height is. The seizure threshold is also lower in infants compared to older children and adults.
HHV-6 is the most frequently implicated viral infection in the US, likely due to the high fevers which are the hallmark of the infection.
Genetics likely plays a role, but given that this is an ED reference and not a pediatric or genetics reference guide, we frankly aren’t interested in delving into that and we are sure you would thank us.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Definitions (6)
Accepted criteria of febrile seizures include the following:
-Convulsion in the setting of a temperature >38 C
-Child older than 6 months but younger than 5 years
-No central nervous system infection of inflammation
-No metabolic abnormalities
-No previous afebrile seizures
Classification (7-9)
We further divide febrile seizures into simple and complex. This has implications for board questions and for practice decision making.
Simple febrile seizures: the majority of febrile seizures. Generalized, <15 minutes, one in 24 hours. Children return to baseline quickly.
Complex febrile seizures: Less common overall. If any of the following are present, its considered a complex seizure: focal onset, >15 minutes, or more than one in 24 hours.
Those with complex febrile are more likely to be younger and have abnormal development.
Patients with complex seizures have a higher risk of recurrent febrile seizures and a higher risk of future nonfebrile seizures.
Presentation (10)
The child must have a fever. Any fever will do, but it is typically found >39 C.
Often, the seizure is the first indication that the child is ill to the parents.
It is often difficult in infants to clearly tell a seizure has ablated. Important clues include presence of closed eyes and a deep breath. Children with open eyes and a stare or lip smacking might still be seizing even without convulsive activity.
Postictal phase is associated with drowsiness, confusion, and rarely agitation.
Prolonged drowsiness is concerning for other etiologies (e.g. meningitis, brain mass, encephalitis).
Transient hemiparesis (Todd paralysis), is extremely rare (<2% of all cases).
Physical exam should be thorough and include neurological assessment, assess for meningismus, bulging fontanelle, and note differences in muscle movement or strength.
Look for an obvious source of infection- throat and ears in age-appropriate children.
Differential Diagnosis: what about meningitis?
Epilepsy, CNS pathology (meningitis, abscess, encephalitis, VP shunt complication, brain mass).
Want to hear a frightening statistic?
As many as 40% who have seizures as initial manifestation of meningitis have no other meningeal signs. Fever and prolonged recovery with altered mental status are typically the only clues.
However, this does not mean you need to do LPs on everyone. Indeed, it is very rare for bacterial meningitis to be found on the basis of CSF evaluation alone. In fact, when the only indication for performing LP is seizure, meningitis is found in <1% of patients, less than half of those have bacterial meningitis.
On a lighter note, rigors, or shaking chills, can be confused with seizures. A detailed history is critical to tell the difference. Chills rarely involve facial muscles, do not cause loss of consciousness, and are non-focal. Chills are suppressible with touch.
Management (11-15)
In children who are at baseline, with a typical history of a simple febrile seizure and a reassuring nonfocal exam, no further diagnostic evaluation is indicated, and only reassurance is warranted.
Fever control is essential in the ED, and antipyretics are first line to reduce temperature and prevent further seizures.
That means don’t get random CBCs, BMPs, glucose sticks, or lactates. These should be ordered if you are actively concerned about an alternative diagnosis.
Neuroimaging is not required and actually causes more harm.
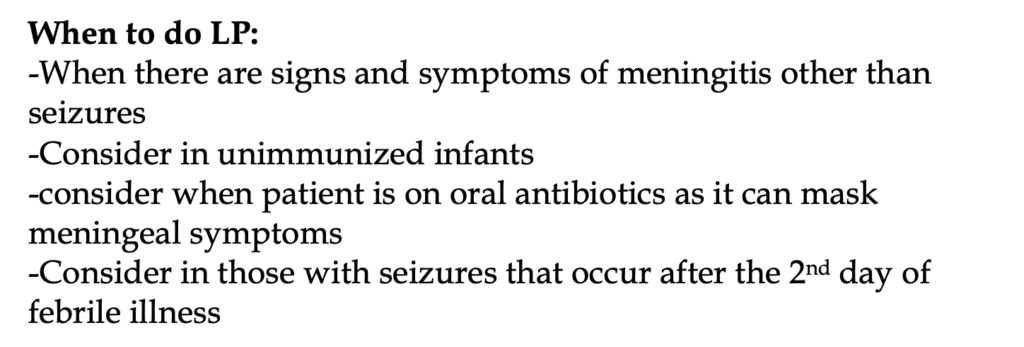
LP is unnecessary in well-appearing children who are at baseline after a febrile seizure.
Children presenting with a complex febrile seizure, especially if it is their first, require a deeper approach as underlying etiologies are more common and there is a small, but increased risk of future afebrile seizures.
EEG and MRI might be needed in the future but are not typically warranted in the acute setting.
What if the child enters febrile status epilepticus?
This is a rare occurrence, and many authors disagree on what exactly to do. Focus on the basics, ABCs first, and if antipyretics and benzodiazepines fail, anticonvulsants might be needed.
These patients are more likely to have a family history of epilepsy as well as a more defined viral or bacterial illness.
References
1. Millichap JG. The definition of febrile seizures. In: Febrile Seizures, Nelson KB, Ellenberg JH (Eds), Raven Press, New York 1981.
2. Berg AT, Berkovic SF, Brodie MJ, et al. Revised terminology and concepts for organization of seizures and epilepsies: report of the ILAE Commission on Classification and Terminology, 2005-2009. Epilepsia 2010; 51:676.
3. Millichap JG. Febrile Convulsions, Macmillan, New York 1968.
4. MILLICHAP JG. Studies in febrile seizures. I. Height of body temperature as a measure of the febrile-seizure threshold. Pediatrics 1959; 23:76.
5. Hall CB, Long CE, Schnabel KC, et al. Human herpesvirus-6 infection in children. A prospective study of complications and reactivation. N Engl J Med 1994; 331:432.
6. Subcommittee on Febrile Seizures, American Academy of Pediatrics. Neurodiagnostic evaluation of the child with a simple febrile seizure. Pediatrics 2011; 127:389.
7. Nelson KB, Ellenberg JH. Predictors of epilepsy in children who have experienced febrile seizures. N Engl J Med 1976; 295:1029.
8. Hesdorffer DC, Benn EK, Bagiella E, et al. Distribution of febrile seizure duration and associations with development. Ann Neurol 2011; 70:93.
9. Berg AT, Shinnar S. Complex febrile seizures. Epilepsia 1996; 37:126.
10. Millichap JG. Febrile Convulsions, Macmillan, New York 1968.
11. Oluwabusi T, Sood SK. Update on the management of simple febrile seizures: emphasis on minimal intervention. Curr Opin Pediatr 2012; 24:259.
12. Green SM, Rothrock SG, Clem KJ, et al. Can seizures be the sole manifestation of meningitis in febrile children? Pediatrics 1993; 92:527.
13. Guedj R, Chappuy H, Titomanlio L, et al. Risk of Bacterial Meningitis in Children 6 to 11 Months of Age With a First Simple Febrile Seizure: A Retrospective, Cross-sectional, Observational Study. Acad Emerg Med 2015; 22:1290.
14. Kimia AA, Capraro AJ, Hummel D, et al. Utility of lumbar puncture for first simple febrile seizure among children 6 to 18 months of age. Pediatrics 2009; 123:6.
15. Thoman JE, Duffner PK, Shucard JL. Do serum sodium levels predict febrile seizure recurrence within 24 hours? Pediatr Neurol 2004; 31:342.