Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewers: Travis Smith, DO; Mary Claire O’Brien, MD
Introduction
Hypoglycemia is very uncommon in individuals who do not have insulin-treated diabetes. By far, most cases of hypoglycemia occur in the setting of diabetic management. Other causes (in diabetics and non-diabetics) include medications, accidental/intentional hypoglycemia, hormonal deficiency, illicit drugs, alcohol, those critically ill from sepsis, adrenal insufficiency, a non-islet cell tumor, and prior Roux-en-Y gastric bypass surgery.1
Presentation
Hypoglycemia just might be the greatest mimicker in medicine. Basically. no symptom is off-limits to hypoglycemia. Autonomic symptoms are often described, including diaphoresis, palpitations, anxiety, and tremors, as well as neurologic symptoms like numbness, weakness, headaches, mental status change, dizziness, and even seizures.2,3
The lower limit of a fasting plasma glucose is 70 mg/dL in males, 60 mg/dL in females. Most patients develop symptoms when glucose levels <55 but remember that anyone can develop symptoms of hypoglycemia at any point in time.
In short, suspect hypoglycemia in any patient with unexplained unconscious or semiconscious state, or with any neurologic complaint.
Never forget these drugs that cause hypoglycemia:
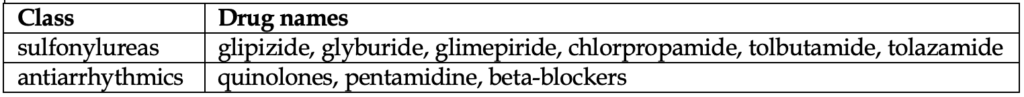
Aren’t there others? Yes, plenty. Basically, every diabetic agent ever made (yes even metformin). Do you need to memorize that? No, don’t bother. The one exception are the sulfonylureas. We put them in the table above because you cannot forget about them. They can cause prolonged, recurrent hypoglycemia, and can be deadly. Never discharge these patients after correcting their glucose levels. You’ll likely need to give IV dextrose and octreotide (more on that later) and admit for monitoring as you would with hypoglycemia from long-acting insulin.
You should be asking diabetic patients about their average glucose levels at home, most recent medication/insulin regimen taken, and recent food intake.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Diagnosis
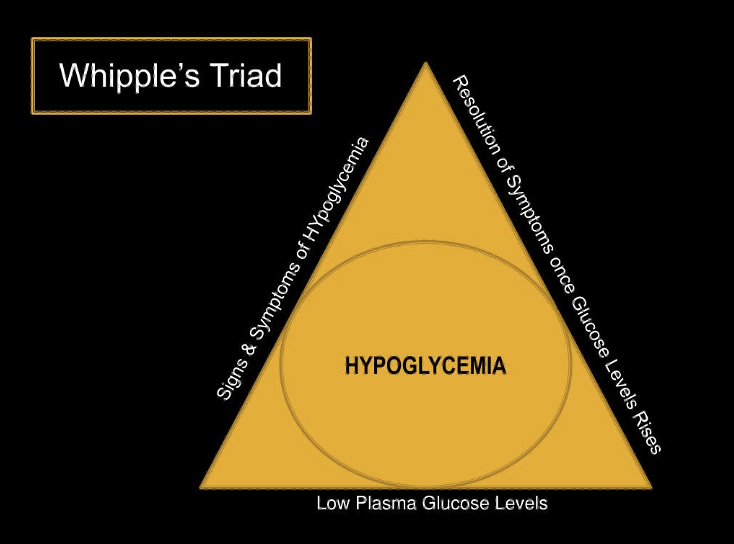
This may seem obvious, but there is a triad to diagnose non-diabetics with symptomatic hypoglycemia, and yes, it is common sense. It’s called the Whipple Triad:
– symptoms of suspected hypoglycemia
– low plasma or fingerstick glucose
– resolution or vast improvement after glucose level is raised
For diabetic patients, all you need is a glucose ≤ 70 to diagnose hypoglycemia.
Management
Asymptomatic: re-measure the level in ~20-30 minutes. If it lowers further, give the patient something to eat. If it is unchanged, no action is indicated.
Symptomatic:
Patient can tolerate PO: Obviously this is preferred (e.g. small juice cup or small soda, 4-5 saltine crackers, 6-8 hard candies). Retest the patient in 15 minutes. If glucose is still low, give a meal/bigger snack to the patient.
Patient cannot tolerate PO:
No IV access: Glucagon is usually readily available in your ED or on the ambulance in the field. Giving intramuscular glucagon immediately is preferred to waiting and attempting IV access. Glucagon can be given subcutaneously, nasally, or intramuscularly. Side effects of glucagon include nausea, vomiting, and sweating.
Glucagon is quite effective, with patients usually becoming less symptomatic in 15 minutes. Follow up with PO intake if patient can tolerate.
IV or IO access: dextrose therapy. There’s a lot of misinformation about this so let’s clear it up. You have two choices: D50 or D10.
Concentrated IV Dextrose 50% (D50) provides 25g of dextrose in a 50 mL bag or syringe (1 ampule).
■ It should be given slowly over 1-3 minutes, not slammed. D50 can extravasate and cause thrombophlebitis.
■ D50 boluses may cause rebound hypoglycemia, so you will likely need to start IV D5W after.
■ D50 can overshoot and cause hyperglycemia, which is bad for critically ill patients but likely not a big deal in the more common causes like accidental hypoglycemia from too much insulin or someone forgetting to eat after taking their routine dosing.4
D10 commonly comes in 10g/100mL and is given as a 100 mL bolus.
■ it has a lower osmolarity and has several advantages.
■ can be easily given peripherally and less likely to extravasate.
■ more likely to safely increase blood sugar levels without overshooting and causing hyperglycemia.5
After the initial correction, PO tolerant patients need to eat, PO intolerant might need a dextrose drip (i.e., D5W at 75-100 mL/hr).
Octreotide (50-150mcg every 6 hours) should be given to those patients whom sulfonylurea overdose is suspected.
Disposition
Any hypoglycemic patient with suspected long-acting insulin usage or sulfonylurea ingestion needs to be admitted and watched for a minimum of 24 hours.
Diabetic patients not taking sulfonylureas or on long-acting insulin: discharge is appropriate if their BMP is normal with close PCP follow-up after a short observation in the ER. Don’t forget insulin education.
In nondiabetic patients who are not critically ill, think about medication interactions, alcohol abuse, sepsis, cortisol deficiency, or malnutrition. Consider “food access” in elderly patients who live alone and who may have trouble with ADLs, including cooking for themselves. These patients may do well “in hospital” when their diet is provided only to become hypoglycemic after discharge.
Patients don’t often develop hypoglycemia randomly and may need admission due to underlying pathology.
References:
1. Cryer PE. Hypoglycemia in Diabetes. Pathophysiology, Prevalence, and Prevention, 3rd ed. American Diabetes Association. Alexandria 2016
2. Hepburn DA, Deary IJ, Frier BM, et al. Symptoms of acute insulin-induced hypoglycemia in humans with and without IDDM. Factor-analysis approach. Diabetes Care 1991; 14:949.
3. Cryer PE. Hypoglycemia, functional brain failure, and brain death. J Clin Invest 2007; 117:868.
4. Spaulding A. D50 vs D10 for severe hypoglycemia in the emergency department. Academic Life in Emergency Medicine. 2014. Available from: https://www.aliem.com/2014/d50-vs-d10-severe-hypoglycemia-emergency-department/
5. Kiefer M, Hern H, Alter H, et al. Dextrose 10% in the treatment of out-of-hospital hypoglycemia. Prehosp Disaster Med. 2014;29(2):190-4.


