Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Edan Zitelny, MS3, Blake Briggs, MD
Peer reviewer: Mary Claire O’Brien, MD
Introduction
DKA is one of the most serious acute complications of diabetes mellitus (DM). It can occur in both Type I and Type II DM as well as gestational DM, with the highest prevalence seen in patients with Type I DM. DKA should be treated as a medical emergency, as delaying management can end choco-terribly (get ready for some sugary puns!). DKA has a 10-20% mortality rate, HHNS is 10x higher.
Hyperosmolar hyperglycemic nonketotic syndrome (HHNS) is a similar condition to DKA, but more common in T2DM. It is a condition of profound hyperglycemia leading to altered mental status, dehydration, and acidosis.
In short, DKA = disease of no insulin, HHNS = disease of insulin resistance.
Pathophysiology
Disease is often secondary to insulin deficiency or resistance coupled with glucagon excess. If there is other underlying inflammatory process, catecholamine and cortisol release often opposes insulin further. This combination often contributes to accelerated hyperglycemia and ketogenesis. The degree of hyperglycemia seen often drives osmotic diuresis leading to dehydration and volume depletion leading to electrolyte abnormalities and their corresponding sequelae.
The distinction between HHNS and DKA is not often readily apparent in the ED, and for the most part it doesn’t matter because the treatment is the same: insulin drip, fluid resuscitation, and closely managing electrolytes.
The boards only test on the epidemiologic differences between HHNS and DKA, so enjoy that. Let’s help clarify the candy:
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Presentation
Patients in DKA will often present with nonspecific symptoms, including N/V and generalized abdominal pain. Rarely, there is a fruity breath odor (secondary to acetone development or just lots of Gushers). Patients will often complain of the “Poly’s” – polydipsia, polyuria, and polyphagia.
Patients will ALWAYS be significantly fluid depleted (may see orthostatic hypotension, tachycardia, skin tenting, etc.).
Classically for board exams, Kussmaul respiration (fancy way to describe rapid, deep breathing) can be seen in severe cases, secondary to severe metabolic acidosis.
Diagnosis
The classic criteria for diagnosis of DKA is threefold:
- Hyperglycemia (usually between 350-500 mg/dL, with value often <800 mg/dL)
- Anion gap metabolic acidosis (confirmed with ABG/VBG, usually with pH < 7.30 or serum bicarbonate <15)
- Positive serum/urine ketones (confirmed with UA or specific ketone test including acetoacetate, acetone, and β
hydroxybutyrate)
DKA patients are often hyponatremic, with profound ketonemia and ketonuria. DKA rapidly develops <24 hours.
Criteria for HHNS include: Diabetic patient with AMS, Severely elevated glucose (usually >600), Minimal ketonuria or ketonemia, Serum osmolality >320, Bicarbonate >15, or pH >7.3
HHNS is another way of saying hyperglycemia + dehydration leading to altered mental status (AMS). Patients are classically older, more likely to be type 2 diabetics, and nursing home residents.
AMS can be generalized or have focal neurologic deficits. AKI is common. Unlike DKA, it develops over days/weeks with minimal to no ketoacidosis.
Patients are often pseudohyponatremic, hypomagnesemic.
Most importantly, HHNS patients have more of a fluid deficit- incredibly often >100 mL/kg!
Thromboembolic events more common in HHS (due to hyperviscosity), and there is a 10x higher mortality than DKA.
There is a distinct correlation with changes in Mental status and serum osmolarity.
Causes of both HHNS and DKA
DKA is often a consequence of stress on the body. The classic mnemonic to remember is The 5 I’s of DKA:
- Infection
- Infarction
- Insemination
- Insulin (noncompliance)
- Initiation (first time T1DM presentation)
Important differential diagnoses:
Alcoholic ketoacidosis (anion gap metabolic acidosis without significant hyperglycemia)
Hypoglycemia (altered mental status, abdominal pain, and acidosis; fairly obvious on initial fingerstick). Sepsis (sepsis should be suspected in patients with hyperglycemia and fever)
Other things to think about: Intoxication (e.g. methanol, ethanol, salicylates, isopropyl alcohol, paraldehyde, ethylene glycol)
Work-Up
After a routine H&P and ABC’s, you should order a stat blood glucose. The glucose >250 in the setting of correct presentation should prompt investigation for DKA/HHNS. This includes venous blood gas, CBC, BMP, and urine analysis with urine pregnancy test.
In adult patients, EKG should be performed if there is concern for cardiac ischemia as a cause. We do not routinely do CXR or blood cultures unless patients are febrile or there is a large concern for infection as a cause.
Treatment
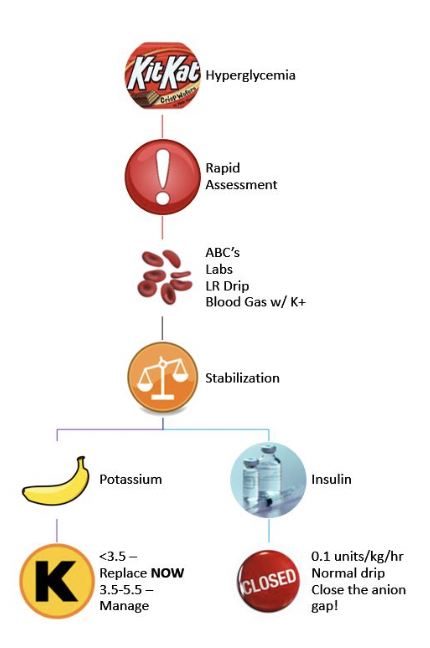
IV access is crucial, as the first intervention is starting IV crystalloid boluses, LR vs NS. We prefer LR, see our podcast, episode 24 on “LR vs NS” for why.
The goal of fluids is to correct both hypovolemia and hyperosmolality. Most patients are profoundly dehydrated, and we administer rapid fluid boluses while awaiting further lab studies before starting insulin. Once fluid is running, correcting the sugar becomes the next priority, which is achieved with IV regular insulin at 0.1 units/kg/hr to tame glucose and close the anion gap. Be certain that the patient is not hypokalemic before giving insulin. Insulin boluses have fallen out of style as they studies in adults have found neither significant benefit nor harm from using an insulin bolus. There might be risk of cerebral edema in children. However, a pro-move in the ED while you are waiting for the insulin drip (if it takes a while), is to inject 10U regular insulin IV push if you find yourself waiting for a long time for the drip. When the drip is started be aggressive about increasing it fast if no rapid improvement.
After a few hours, fluid replacement and insulin administration depends more on the clinical presentation/state of hydration, serum electrolyte levels, and I/O’s. Maintenance LR is what we prefer (we belong to the House of Ringers Lactate).
The key electrolyte to evaluate is potassium! Replacement should be initiated immediately if <3.5 mEq/L. Almost all patients have a substantial potassium deficit, usually due to urinary losses generated by glucose osmotic diuresis. The only reason K+ is elevated on presentation is because of the acidosis.
If K+ between 5.5-3.5 mEq/L, 20-30 mEq of KCl should be given along with insulin via IV fluids due to cellular shifts seen with introduction of insulin. While the Na+ may look uncharacteristically low, like the K+, it is typically due to pseudohyponatremia (glucose replaces Na as the main ion of the blood). Hyponatremia often requires no treatment, and we recommend close monitoring for improvement as treatment progresses.
When glucose reaches ~250 mg/dL, we advise switching to IV fluids that contain dextrose.
Bicarbonate? Na-HCO3 has not been found to decrease mortality or morbidity. What patients need is maximally aggressive management of their DKA (fluids and more insulin).. There is no evidence that bicarbonate works as a treatment of ketoacidosis.Do not give if pH >6.9. If pH is below this and patient is in extremis, giving 100 mEg might not be a bad idea, but there is minimal evidence for it. In fact, raising bicarbonate levels in theory will reduce respiratory drive and possibly worsen the metabolic acidosis. This whole area is controversial, and we advise no bicarbonate unless pH <6.9 and the patient is clinically in extremis (not sitting up in bed and talking).
Resolution— The hyperglycemic crisis is considered to be resolved when the following goals are reached:
- Ketoacidosis has resolved: normalization of the serum anion gap (less than 14 mEq/L) and blood beta-hydroxybutyrate levels undetectable.
- The patient is able to eat.
Once the patient is able to eat after the ketoacidosis resolves, switching to subcutaneous insulin schedule with IV insulin infusion overlap is preferred. This likely won’t happen in the ED but if it does then you probably have some serious admission issues. While in the ED, hourly blood glucose sticks and 2-4-hour BMPs should be performed.
Disposition
A DKA/HHNS patient on an insulin drip should be admitted to the ICU or a very closely monitored intermediate unit. If the drip is off, floor is probably fine.
Complications
Hypoglycemia and hypokalemia are by far the most common complications of the treatment of DKA and HHNS.
Cerebral edema is the scary rare complication to worry about in DKA, and it’s the complication that will be tested on. Its insanely rare, occurring in <1% of all DKA patients, but mortality is up to 90% in children alone. Symptoms typically emerge within 12-24 hours from the initiation of treatment. Headache is the earliest clinical manifestation, followed by lethargy and decreased arousal. Neurologic deterioration is rapid. Seizures, incontinence, pupillary changes, bradycardia, and respiratory arrest can develop. The rate of progression to brainstem herniation may be so rapid that clinically recognizable papilledema does not develop.
Treatment: Mannitol. Act fast. Steroids and diuretics are wrong answers and have no role.
References:
- American Diabetes Association: Hyperglycemic crises in patients with diabetes mellitus (Position Statement). Diabetes Care 24:1988–1996, 2001
- Driver BE et al. Discharge glucose is not associated with short-term adverse outcomes in emergency department patients with moderate to severe hyperglycemia. Ann Emerg Med 2016
Dec; 68:697.
- Basu A, Close CF, Jenkins D, Krentz AJ, Nattrass M, Wright AD: Persisting mortality in diabetic ketoacidosis. Diabet Med 10:282–289, 1992
- Bello FA, Sotos JF: Cerebral oedema in diabetic ketoacidosis in children.Lancet 336:64, 1990
- Boyd JC et al. Relationship of potassium and magnesium concentrations in serum to cardiac arrhythmias. Clin Chem 1984; 30(5): 754-7. PMID: 6713638
- Ennis ED, Stahl EJVB, Kreisburg RA: The hyperosmolar hyperglycemic syndrome. Diabetes Rev 2:115–126, 1994
- Gerich JE, Martin MM, Recant LL: Clinical and metabolic characteristics of hyperosmolar nonketotic coma. Diabetes 20:228–238, 1971
- Guisado R, Arieff AI: Neurologic manifestations of diabetic comas: correlation with biochemical alterations in the brain. Metabolism 24:665–669,1975
- Kaufman FR, Halvorson M: The treatment and prevention of diabetic ketoacidosis in children and adolescents with type 1 diabetes mellitus. Pediatr Ann 28:576–582, 1999
- Kitabchi AE, Ayyagari V, Guerra SMO, Medical House Staff: The efficacy of low dose versus conventional therapy of insulin for treatment of diabetic ketoacidosis.Ann Int Med 84:633–638, 1976
- Kitabchi AE, Umpierrez GE, Murphy MB, Barrett EJ, Kreisberg RA, Malone JI, Wall BM: Management of hyperglycemic crises in patients with diabetes. Diabetes Care 24:31–53, 2001
- Morris LR, Kitabchi AE: Efficacy of low-dose insulin therapy for severely obtunded patients in diabetic ketoacidosis. Diabetes Care 3:53–56, 1980



