Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Salar Rafieetary, MD
Peer editor: Blake Briggs, MD
Dr. Salar Rafieetary is a first year Vitreoretinal Surgery fellow at the Charles Retina Institute in Memphis, TN. He completed his medical school at UTHSC, graduating as an AOA member, GHHS member, as well as class president all four years. He completed his residency at UTHSC Hamilton Eye Institute.
Introduction 1-5
A posterior vitreous detachment (PVD) is defined as a separation between the posterior vitreous cortex and the internal limiting membrane (ILM) of the retina. The frequency of PVD varies based on multiple risk factors, most importantly age, female gender, and degree of myopia (nearsightedness). Other reported risk factors have been trauma, intraocular inflammation, and retinal vascular diseases, higher intake of Vitamin B6, and presence of collagen synthesis disease (i.e. Stickler syndrome, Marfan Syndrome). Age- related PVD occurs due to progressive liquefaction of the vitreous, seen in 50% of people over age 70, plus progressive weakening of the vitreoretinal adhesion.
Complications of PVD include retinal tear, vitreous hemorrhage, rhegmatogenous retinal detachment, and retinal and/or disc hemorrhage. The pathophysiologic mechanism of these complications is caused by vitreous traction on focal areas of the retina or optic nerve. Formation of a full thickness retinal break is the most common complication, occurring in approximately 8-10% of patients with an acute PVD. A full thickness retinal break, if not diagnosed and treated with laser or cryotherapy can result in a rhegmatogenous retinal detachment.
Brief anatomy 3
Vitreous is a clear gel-like structure that occupies the vitreous cavity of the eye, occupying a volume of approximately 4.0 mL. Vitreous is 98% water and 2% structural proteins and extracellular matrix. Type II collagen is the major structural protein in vitreous. As one ages, liquefaction of the vitreous occurs accompanied by age-related weakening of the adhesions between the posterior vitreous cortex and the ILM.
Presentation 2, 6-8
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Symptoms of a PVD include seeing floaters, flashes of light, or both. If a PVD causes a vitreous hemorrhage, the patient will often report a painless decrease in vision and dense floaters.
The differential diagnosis for a patient presenting with complaint of floaters includes vitreous hemorrhage (which may be secondary to diabetic retinopathy or other vasculopathy or can occur from a PVD), vitritis (usually associated with eye redness, +/- eye pain, presence of anterior segment inflammation, history of systemic autoimmune or infectious disease) or migraine (typically lasts 20 minutes and may or may not be associated with headache).
You must ask the patient about timing (sudden onset vs. slow onset), recent trauma, recent ocular surgery (i.e. cataract surgery), presence or absence of headache (associated with migraine), presence of absence of eye pain and redness (associated with vitritis), and personal or family history of retinal detachment.
Physical exam: Visual acuity must be checked objectively with a Snellen chart, ideally with the patient’s glasses or contact prescription. If the patient does not have their glasses or contacts, a pinhole can be very helpful to more accurately measure visual acuity.
Pupils must be examined to rule out presence of a relative apparent pupillary defect (RAPD), which can be seen in macula involving retinal detachments.
The patient must have a dilated eye exam by an ophthalmologist or optometrist. A meta-analysis of patients with symptomatic PVDs reported an 8.2% incidence of retinal tears. In a series of 39 patients with symptomatic retinal tears, 32 had retinal tears without surrounding retinal detachment. Without intervention with laser or cryotherapy, 31% of these patients developed a subsequent retinal detachment. This highlights the importance for a dilated eye exam by an experienced clinician.
If your ED does not have access to an on-site ophthalmologist or optometrist, arrangements should be made for outpatient follow-up the next day.
In the ED, a useful tool is POCUS. Ultrasound can be helpful to diagnose a PVD and rule out a retinal detachment. A single blinded study of emergency physicians with varying ultrasound experience revealed a 74.6% and 85.7% success rate of diagnosing retinal detachment and PVD using POCUS. While POCUS is a useful tool in the ED, it does not replace the need for a thorough dilated eye exam by an experienced ophthalmologist or optometrist.
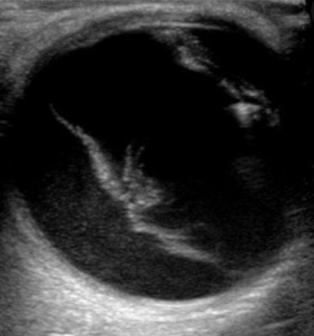
The findings on POCUS for retinal and PVD are similar. Both clearly have detachment of a membranous surface from the posterior wall of the eye. However, PVD will not be tethered to the optic disc (see right).
Management
No treatment is indicated for a PVD. If a retinal break is identified by an eye care provider, referral must be made to a retina specialist for treatment with laser or cryotherapy.
Patients should be educated on the symptoms of a retinal detachment, including increase in floaters, flashing lights, a curtain or shadow in the field of vision. Presence of any of these symptoms warrants urgent presentation to the ED or to a retina specialist.
References:
1. Johnson MW. Posterior vitreous detachment: evolution and complications of its early stages. Am J Ophthalmol. 2010;149(3):371-82.e1. doi:10.1016/j.ajo.2009.11.022
2. Bagheri N. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. Philadelphia: Wolters Kluwer; 2017.
3. Schachat AP, Wilkinson CP, Hinton DR, Sadda SVR, Weidemann P. Ryan’s Retina. New York, NY: Elsevier; 2018.
4. Hayreh SS, Jonas JB. Posterior vitreous detachment: clinical correlations. Ophthalmologica. 2004;218(5):333-343. doi:10.1159/000079476
5. Chuo JY, Lee TY, Hollands H, et al. Risk factors for posterior vitreous detachment: a case-control study. Am J Ophthalmol. 2006;142(6):931-937. doi:10.1016/j.ajo.2006.08.002
6. Coffee RE, Westfall AC, Davis GH, Mieler WF, Holz ER. Symptomatic posterior vitreous detachment and the incidence of delayed retinal breaks: case series and meta-analysis. Am J Ophthalmol. 2007;144(3):409-413. doi:10.1016/j.ajo.2007.05.002
7. Davis MD. Natural history of retinal breaks without detachment. Arch Ophthalmol. 1974;92(3):183-194. doi:10.1001/archopht.1974.01010010191001
8. Baker N, Amini R, Situ-LaCasse EH, et al. Can emergency physicians accurately distinguish retinal detachment from posterior vitreous detachment with point-of-care ocular ultrasound?. Am J Emerg Med. 2018;36(5):774-776. doi:10.1016/j.ajem.2017.10.010



