Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer editors: Travis Smith, DO, Mary Claire O’Brien, MD
Introduction
Tricyclic antidepressants (TCAs) have a long history in the management of psychiatric disease, especially depression. Since the arrival of SSRIs and other related medications, TCAs are used much less commonly. Currently, TCAs have been relegated to the treatment of migraines, chronic pain syndromes, insomnia, and other obscure neuropathic/musculoskeletal/somatic disorders.1 TCA poisoning, while uncommon, remains a life-threatening issue and continues to be a classic, frequently tested topic on exams.
Pathophysiology
You need to know how TCAs work and the effects they have on receptors. In an overdose, TCAs antagonize a lot of receptors:2
– central and peripheral muscarinic acetylcholine receptors
– peripheral alpha-1 adrenergic receptors
– histamine receptors
– CNS GABA receptors
– cardiac fast sodium channels (#trouble)
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
TCAs are rapidly absorbed in the GI tract and quickly enter systemic circulation within a few hours. They are lipophilic, highly bound to plasma, and therefore have a large volume of distribution.2 They are also metabolized in the liver by CYP2D6 (the same bad actor that metabolizes codeine and tramadol aka “tramdont”) and renally excreted. The scariest of TCA overdose complications is cardiac conduction disruption. The inhibition of Na-fast channels decreases conduction velocity, increases repolarization, and prolongs refractory periods.
This pattern is extremely similar to the Class 1a antiarrhythmics (i.e. quinidine and procainamide).
Presentation
TCA overdose patients classically present with altered mental status– specifically, sedation. Symptoms usually appear around 30 minutes to 2 hours post-ingestion with toxicity lasting for 24-48 hours (with case reports up to five days following a significant amitriptyline overdose). If no symptoms are apparent after 6 hours, then a toxic ingestion is unlikely. In those who are symptomatic, expect signs of anticholinergic toxicity given TCAs’ inhibition of muscarinic receptors (hyperthermia, dilated pupils). They could be hypotensive as well (due to inhibition of alpha-1 receptors and cardiac channels, resulting in vasodilation and decreased contractility, respectively).3,4,5
The course of TCA toxicity can be unpredictable, with patients presenting initially after ingestion with no symptoms, only to rapidly deteriorate. Ingestion of 10-20 mg/kg leads to significant toxicity.6
The three major systems affected by TCAs with their resulting symptoms are described further below:
Anticholinergic toxicity: hyperthermia, flushing, dilated pupils. Patients may have urinary retention.
Cardiovascular toxicity: sinus tachycardia, with progression to hypotension and more cardiac conduction abnormalities. Ventricular tachycardia and ventricular fibrillation occur in ~4% of TCA overdose cases.7
Neurologic toxicity: changes in mental status, usually somnolence, are common. Delirium due to anticholinergic toxicity can less commonly occur. Seizures are a hallmark of an overdose and are associated with worsening cardiac decline.8,9
Diagnosis
Clinical evaluation (including the history and physical exam) combined with classic EKG findings make the diagnosis.
As usual, a general toxicologic workup should occur in the ED, which includes asking EMS or family members about other home medications, as well as other prescription medications found in the household.
Make sure to ask the following: Specific agent, the amount ingested, time of ingestion, any co-ingestions.
Law enforcement might have to be utilized to go to the patient’s place of residence to acquire the medication bottles if the patient is incapacitated or not being forthright. Calling the patient’s pharmacy or any helpful EMR retrieving tricks can pay dividends.
Common toxicologic tests to grab include salicylate and acetaminophen level, CBC, CMP, pregnancy test, on a basic level.
An EKG should be immediately obtained and performed hourly for several hours of observation.
Look for any evidence of prolonged QRS >100 msec, abnormal QRS morphology (deep, wide S wave in any anterior lead, I, or aVL), right bundle branch block, or in general any signs of a “Brugada-like” pattern.10 Also, be on the lookout for an R/S ratio in aVR of ≥0.7,
and an R wave in the aVR lead ≥3 mm. The finding of any one of these changes are indications for IV sodium bicarbonate therapy.
The most important EKG finding is QRS duration >100 msec. Increasing length of the QRS >100 is associated with a higher risk of seizures and ventricular arrhythmias when the QRS duration >160 msec .11, 16
Qualitative urine measurements of TCAs are not helpful in the acute setting. They do not test drug “levels.” They only indicate use, not overdose, and they are not available in the emergency time frame to significantly help patients.
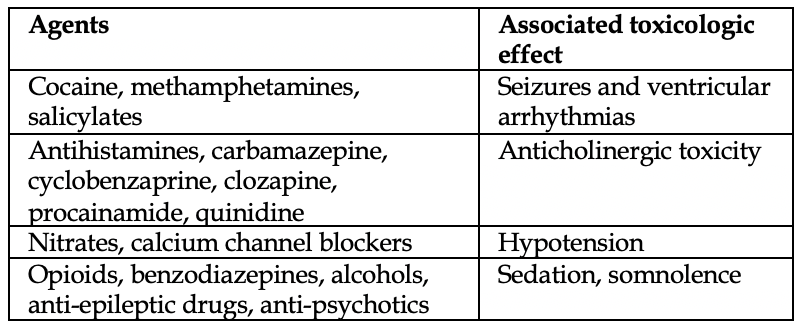
A variety of different toxicologic presentations can be present in a similar fashion. Check out Figure 1 for a solid differential diagnosis list.
TCAs are unique in that no other drug causes such a constellation of overdose pathology (hypotension, arrhythmias, sedation, and seizures).12
Decontamination
We understand this is not commonly used in clinical practice. It is difficult to establish an accurate time of ingestion, patient cooperation may be an issue, and of course there is concern for airway protection. If presenting within ~2 hours of ingestion, 1 g/kg of activated charcoal may be given. Remember, intubation should never be performed for the sole purpose of giving charcoal.13,14
Management
It always starts with ABCs. Many of these patients require intubation, so be very cautious in those with arrhythmias and those who are hypotensive. Address the blood pressure and any potential arrhythmias prior to intubation, if possible.
As with most toxicologic presentations, IV fluids for hypotension (we like lactated Ringers) and IV benzodiazepines for seizures are great choices. Whatever you do, never give physostigmine in TCA overdose. It is associated with cardiac arrest, and that’s not good.
Sodium bicarbonate is the standard of care and is absolutely indicated in those with a QRS >100 on EKG. Na-bicarbonate acts by increasing serum pH and increasing extracellular sodium which likely restores the peace during Phase 0 depolarization. Both make the TCA less available to bind to sodium channels.
The dose is 150 mL of 8.4% sodium bicarbonate (50 mL each syringe), given as a rapid IV push. If there is no response in 5 minutes, a 2nd dose of 150 mL should be given.
Serial EKGs should be performed to evaluate for QRS lengthening and improvement.
A maintenance drip should be started after boluses of Na-bicarbonate accomplish QRS narrowing. 150 mEq of sodium bicarbonate in 1L D5W infused at 250 mL/hour in adults is appropriate. The drip will be tapered over hours to days.
You need to watch for side effects of prolonged Na-bicarbonate therapy: volume overload, hypernatremia, hypokalemia, and metabolic alkalosis. pH measurements should take place hourly until they are normal.
What about patients who do not respond to Na-bicarbonate? Well, that’s unfortunate because there aren’t many other options. Lipid emulsion therapy has been used in a few cases, but there are no clear indications other than unstable patients who do not respond to “standard therapies”. Obviously, consultation with a toxicologist is needed.15
There is no clear data supporting the use of cardiac pacing, ECMO, plasma exchange, or mechanical hemodynamic support.
References
1. Wong J, Motulsky A, Abrahamowicz M, et al. Off-label indications for antidepressants in primary care: descriptive study of prescriptions from an indication based electronic prescribing system. BMJ 2017; 356:j603.
2. Franssen EJ, Kunst PW, Bet PM, et al. Toxicokinetics of nortriptyline and amitriptyline: two case reports. Ther Drug Monit 2003; 25:248.
3. Lynch R. Tricyclic antidepressant overdose. Emerg Med J 2002; 19:596.
4. Kerr GW, McGuffie AC, Wilkie S. Tricyclic antidepressant overdose: a review. Emerg Med J 2001; 18:236.
5. Biggs JT, Spiker DG, Petit JM, Ziegler VE. Tricyclic antidepressant overdose: incidence of symptoms. JAMA 1977; 238:135.
6. Liebelt EL. Chapter 73: Cyclic antidepressants. In: Goldfrank’s Toxicologic Emergencies, 9th ed, Nelson LS (Ed), McGraw-Hill, New York 2011.
7. Goldberg RJ, Capone RJ, Hunt JD. Cardiac complications following tricyclic antidepressant overdose. Issues for monitoring policy. JAMA 1985; 254:1772.
8. Ellison DW, Pentel PR. Clinical features and consequences of seizures due to cyclic antidepressant overdose. Am J Emerg Med 1989; 7:5.
9. Taboulet P, Michard F, Muszynski J, et al. Cardiovascular repercussions of seizures during cyclic antidepressant poisoning. J Toxicol Clin Toxicol 1995; 33:205.
10. Niemann JT, Bessen HA, Rothstein RJ, Laks MM. Electrocardiographic criteria for tricyclic antidepressant cardiotoxicity. Am J Cardiol 1986; 57:1154.
11. Boehnert MT, Lovejoy FH Jr. Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med 1985; 313:474.
12. Sharma AN, Hexdall AH, Chang EK, et al. Diphenhydramine-induced wide complex dysrhythmia responds to treatment with sodium bicarbonate. Am J Emerg Med 2003; 21:212.
13. Bosse GM, Barefoot JA, Pfeifer MP, Rodgers GC. Comparison of three methods of gut decontamination in tricyclic antidepressant overdose. J Emerg Med 1995; 13:203.
14. Roy TM, Ossorio MA, Cipolla LM, et al. Pulmonary complications after tricyclic antidepressant overdose. Chest 1989; 96:852.
15. Levine M, Brooks DE, Franken A, Graham R. Delayed-onset seizure and cardiac arrest after amitriptyline overdose, treated with intravenous lipid emulsion therapy. Pediatrics 2012; 130:e432.
16. Khalid MM, Waseem M. Tricyclic Antidepressant Toxicity. [Updated 2021 Feb 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430931/



