Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Mary Claire O’Brien, MD
Peer Reviewer: Blake Briggs, MD
Introduction
This document will be covering what you need to know about pelvic fractures. The most common mechanism for pelvic fractures: motor vehicle or motorcycle crashes (43-58%), followed by pedestrian struck (20-22%), and then falls (5-30%).
Pelvic fractures only make up ~3% of all skeletal injuries but their overall mortality is quite high at 10%. Open pelvic fractures comprise only 2-4% of all pelvic fractures, but their mortality rates skyrocket, approaching 50%. Older patients have a bad time; age >60 with significant pelvic fracture predicts the likelihood of bleeding requiring angiography.
Brief review of pelvic anatomy
Think of it as 4 bones: the right and left hip bones, the sacrum, and the coccyx.
When assessing pelvic ring injuries, we should think in terms of pelvic stability. Pelvic stability depends on the integrity of a combination of bones and ligaments. Stable fractures are able to withstand normal physiologic loading without significant displacement over time, whereas unstable fractures tend to displace. In general, fractures and dislocations with displacement of more than 1 cm and injuries that compromise the posterior SI ligaments are often unstable and warrant close attention at initial evaluation.
The posterior SI ligaments are the key vertical stabilizers of the pelvis! Therefore, L5 transverse process fractures should raise your suspicion for pelvic ring instability. The L5 nerve root exits its foramen just below that L5 transverse process then runs posteriorly along the sacrum. So, if the vector of force was in the right direction and of sufficient force to fracture the L5TP, it may have injured the posterior ligament complex, which is critical for stability of the pelvis.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Historically, pelvic fractures have been classified according to whether there is pelvic stability or instability. You do not need to memorize the details of the different classification systems (#thankgod) but should understand that sorting pelvic fractures based on force vectors allows the orthopedic surgeon to apply external fixation in the most appropriate manner to correct pelvic deformity and to maximize patients’ survival.
Specific to the “Young and Burgess” classification currently used is that the pelvic bony injury pattern can predict associated injuries. Head and chest trauma are associated with lateral compression injuries, while visceral injury and hemorrhage are associated with AP compression injuries. It was originally thought that this classification could predict the extent of hemorrhage… but subsequent studies have shown that significant hemorrhage can still occur with even “lesser” fractures.
Pelvic radiography
Let’s talk about trauma codes and initial plain films. Plain films from the initial trauma series has been found to have a low sensitivity (55%) for predicting stability. Repeat: that first x-ray is not reliable in determining whether a pelvic injury is stable.
So, what should we be looking for on those initial pelvic films?
ABCs: alignment, bones, cartilage, soft tissues.
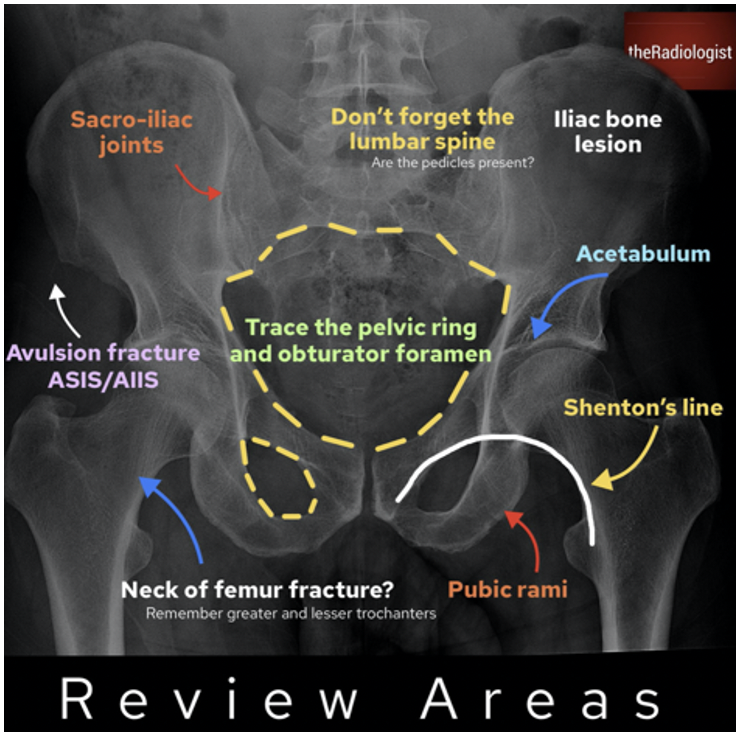
There are anatomical lines of the pelvis on an anteroposterior radiograph as directly pictured above. These lines should be continuous and smooth.
One question that comes up in reviewing AP radiographs is what’s a normal pubic symphysis? The answer is 4-5 mm unless the patient is pregnant. In a pregnant patient, the pubic symphysis may relax up to 9mm.
AP radiographs are helpful for assessing pelvic symmetry and anterior ring, iliac wing, and transverse process fractures. You should look for symmetry of the wings and should compare the obturator foramina.
Specific fractures
Think of these fractures by mechanism.
#1: Lateral compression fractures. Think of an MVC or MCC patient who has been T-boned. Lateral compression fractures are associated with head and chest injuries.
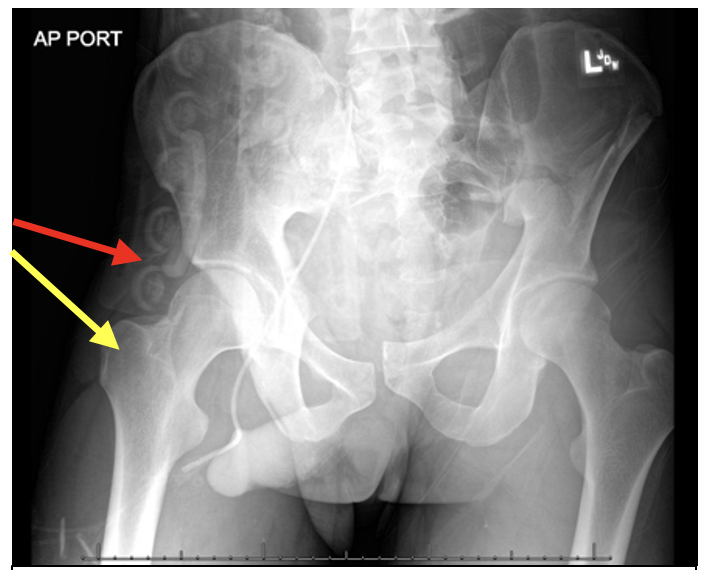
#2: AP Compression fractures are typically from head-on motor vehicle accidents, motorcycle accidents, falls, and crush injuries. They typically produce external rotation of one or both hemipelvises, leading to an “open-book” type of injury. Again: look for symmetry of the iliac wings on your plain films. Remember that AP compression fractures are associated with visceral injuries and hemorrhage. Substantial hemorrhage and arterial bleeding are most prevalent with AP compression injuries, and the severity may be determined on the basis of whether active extravasation is present on arterial phase images or whether a large volume of pelvic hemorrhage is present.
The presence of more than 500 mL of extraperitoneal hemorrhage has been found to correspond with a 50% probability of pelvic arterial injury. AP compression injuries with severed arteries are associated with high rates of morbidity and mortality.
#3: Vertical shear fractures are caused by cranially directed high-energy forces from violent axial loading of the hemipelvis, such as occurs with falls from a height where the patient lands on an extended leg. The exact fracture pattern depends on both the amount of force applied and the relative strength of the bone and ligamentous structures.
#4: Acetabular fractures. A typical case would be a driver in MVC with right hip pain, whose foot was extended on the gas pedal. If there is concern for an acetabular fracture, CT is the best diagnostic modality. Look on the CT if you suspect an acetabular fracture and the plain radiograph is inconclusive.
Presentation
In an alert trauma patient you would expect the obvious here: symptoms like abdominal pain, pelvic pain, hip pain, back pain. Signs of possible pelvic fracture include tachycardia, hypotension, bruising of the flanks, pelvis, or groin, abdominal distention, leg length discrepancy.
Assessment of the pelvis during trauma
True pelvic volume is about 1.5 liters. However, disruption of the retroperitoneum leads to a non-compressible space for hemorrhage to accumulate. On the average, an adult human male who weighs 70 kg has a blood volume of about 5 liters. You can essentially bleed out your entire blood volume, into your pelvis.
Which of the following is the most likely source of hemorrhage in a major trauma patient with pelvic fractures?
It’s the venous plexus. Classically venous hemorrhage accounts for 90% of bleeding from pelvic fractures, and arterial bleeding accounts for only 10%. Hemorrhage due to pelvic fracture remains a major cause of mortality and morbidity in trauma patients.
NEVER rock the pelvis. A gentle lateral to medial palpation with light pressure is all that is needed to check the pelvis for stability.
Pelvic Stabilization
The use of a pelvic stabilizing device (an orthotic, or sheet binding) does NOT seem to limit blood loss in patients with pelvic hemorrhage. It DOES however effectively reduce fracture displacement and decrease pelvic volume. Cadaver studies suggest pelvic binding does not generate sufficient pressures to “tamponade” bleeding. Reduction of pathologic movement/ Prevention of re-injury is probably the most important clinically. Again, never rock the pelvis #guardtheclot!
Pelvic sheet binding is equal to an external fixation device in terms of pelvic stability. Sheets/binders should be centered over the greater trochanters– not the abdomen (see the image below). The goal of binding is “neutral” position; do not over-rotate the unstable pelvis inward—that may exacerbate posterior injury and venous bleeding.
Pelvic angiography
Patients with pelvic fractures and hemodynamic instability or signs of ongoing bleeding after non-pelvic sources of blood loss have been ruled out should be considered for pelvic angiography with embolization. Patients with evidence of arterial intravenous contrast extravasation in the pelvis by CT may require pelvic angiography and embolization regardless of hemodynamic status. Patients older than 60 years with major pelvic fracture (open book, butterfly segment, or vertical shear) should be considered for pelvic angiography without regard for hemodynamic status.
Note that “pre-peritoneal packing” and “external fixation prior to exploratory laparotomy” are institutionally dependent. We have spoken with several orthopedic and trauma physicians elsewhere and this really does vary.
References
◦Khurana B, et al. Pelvic ring fractures: what the orthopedic surgeon wants to know. Radiographics. 2014: Vol. 34, No. 5. https://pubs.rsna.org/doi/10.1148/rg.345135113 Published Online: Sep 10 2014https://doi.org/10.1148/rg.345135113
◦Williams H. Pelvic fractures and associated injuries. https://www.slideserve.com/rex/pelvic-fractures-and-associated-injuries
◦Weatherford B. Pelvic ring fractures. Orthobullets.com. Updated 1/8/2021
◦Nickson C. Pelvic trauma. Life in the fast lane. Nov 3, 2020. https://litfl.com/pelvic-trauma/
◦Lupez, K. Pelvic fractures: ED presentations and management. May 29, 2017. Emdocs.net
◦Uladag N, et al. Anatomic distribution of hematoma following pelvic fracture. Br J Radiol. 2018 May;91(1085):20170840. doi: 10.1259/bjr.20170840.
◦https://www.researchgate.net/figure/Radiographic-images-of-a-79-year-old-woman-with-sacral-insufficiency-fracture-on-the_fig2_282439974
◦Deng F and Skalski M. Pelvic insufficiency fractures. https://radiopaedia.org/articles/pelvic-insufficiency-fractures-1?lang=us
◦Shearer L, Hudson A. Anatomical lines of the pelvis on an anterioposteriorradiograph. BMJ 2014;349:g5047.
◦ White CE, Hsu JR, Holcomb JB. Haemodynamically unstable pelvic fractures. Injury. 2009 Oct;40(10):1023-30. Epub 2009 Apr 16. Review. PubMed PMID: 19371871
◦Nickson C. Weingart on Pelvic Trauma. https://litfl.com/weingart-on-pelvic-trauma/
◦Fracture of the pelvis: Tile classification (original). https://emottawablog.com/2018/01/opening-the-book-pelvic-trauma-in-the-ed/
◦Tile M. Pelvic ring fractures: should they be fixed? J bone Joint Surg [Br] 1988;70-B:1-12. https://doi.org/10.1302/0301-620X.70B1.3276697
◦Burgess AR, et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990 Jul;30 (7): 848-56. doi:10.1097/00005373-199007000-00015. PMID 2381002.
◦Young JW, Burgess AR, Brumback RJ, Poka A. Pelvic fractures: value of plain radiography in early assessment and management. Radiology. 1986;160:445–451.
◦Young JW, Resnick CS. Am J Roentgenol. 1990 Dec;155(6):1169-75. doi: 10.2214/ajr.155.6.2122661.
◦Makky Al Salam H. Acetabular fracture. https://radiopaedia.org/cases/acetabular-fracture-1



