Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Authors: Christopher Musselwhite, MD; Blake Briggs, MD
Introduction
Cervical spine injuries are a commonly tested topic, since 50% of the approximately 17,000 acute traumatic spinal cord injuries involve the cervical spine.1,2 Motor vehicle accidents account for many injuries, followed closely by falls. Not surprisingly, young men, not known for their excellent decision making, make up most of the injuries, but older adults are also at risk after even minor trauma, especially with other risk factors such as osteoporosis or rheumatoid arthritis.
Anatomy
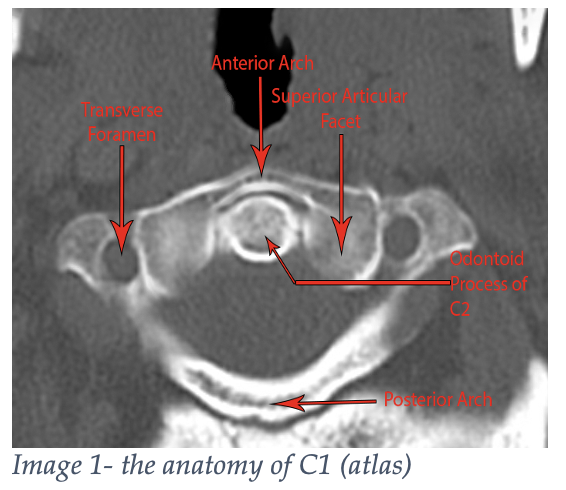
All mammals have seven cervical vertebrae, even giraffes. Birds have 10 to 26- thank goodness we’re not birds.3 The first two cervical vertebrae are unique. The first cervical vertebrae is called the atlas (like Atlas from Greek mythology). This bone is supporting our big globe of a head! As such, the bone has two large lateral masses that articulate with the occipital condyles of the skull but lacks a vertebral body and spinous process (Image 1).
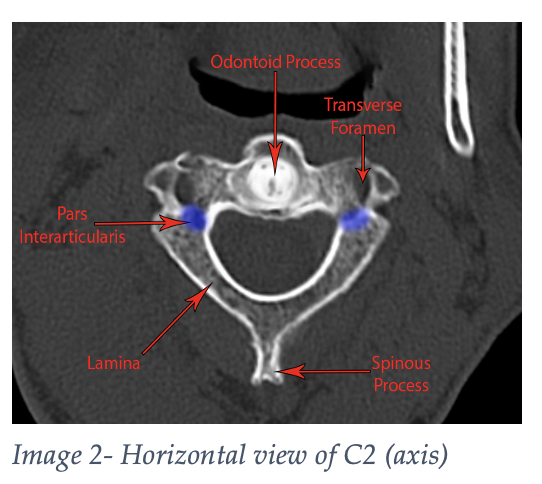
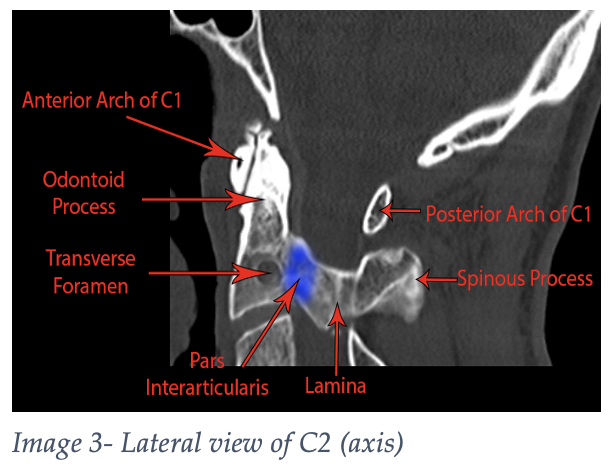
The axis (Images 2 and 3) is the second cervical vertebrae and has a bony process that projects superiorly to the atlas known as the dens, or odontoid process, providing an axis about which the skull can rotate.
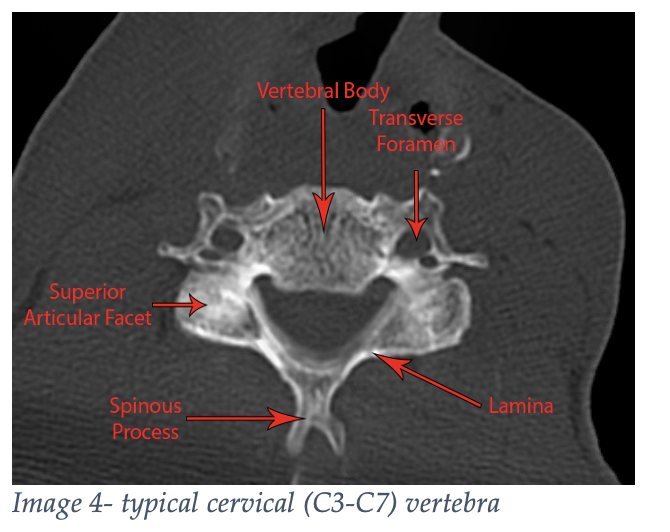
The third through seventh cervical vertebrae all share some common features, such as an anterior vertical body, lateral lamina that merge into a posterior spinous process, making a nice, safe home for the spinal cord (Image 4). The numerous ligaments running up and down the vertebrae bring flexibility and stability.
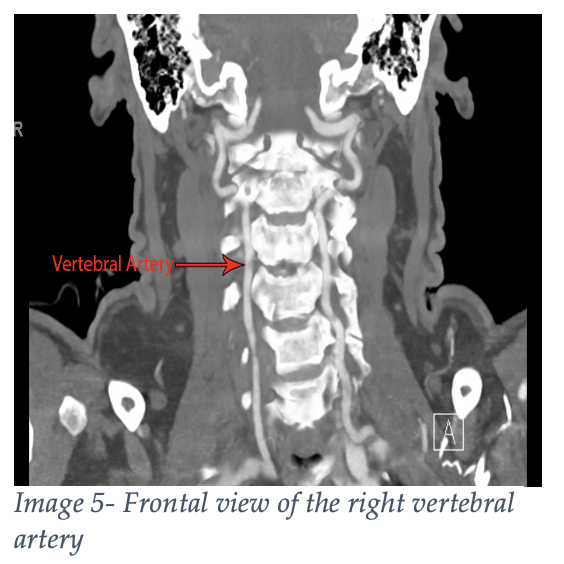
Finally, don’t forget the vertebral arteries passing through the bilateral transverse foramina. Cervical fractures that involve the transverse process or extend into the neural foramina may need angiography to evaluate these arteries at risk.
Unstable Fracture Patterns
Not all fractures are made equal. Some are stable, others…. not so much. Common unstable fracture patterns can be remembered by the mnemonic Jefferson Bit Off A Hangman’s Thumb, standing for Jefferson fracture, Bilateral facet fracture, Odontoid fracture, Atlanto-occipital dislocation, Hangman’s fracture, and Teardrop fracture. Let’s review these for your test. All these fractures will obviously warrant a neurosurgery or spine surgery consult in your ED.
A Jefferson fracture, named after Sir Geoffery Jefferson (what a name!), is a burst fracture of the first cervical vertebrae, the atlas, from axial loading.4,5
The cervical facet joint is part of the postero-lateral spinal canal, where the superior and inferior cervical vertebrae articulate. A bilateral facet fracture is thought to occur with neck hyperflexion primarily, with possible axial loading and/or a rotational component.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
The odontoid can fracture in several different places. A type I dens is through the tip and is generally considered stable, while type II and III are through the base and body respectively and are unstable. This injury can occur with severe hyperextension or hyperflexion.
An atlanto-occipital dislocation can be thought of as internal decapitation. The cranium is attached to the cervical spine with numerous strong ligamental attachments where the occiput meets the atlas. These ligaments can become severed or injured because of a high energy traumatic injury. Since there is a paucity of bony injury, this diagnosis can be difficult to make radiographically. Often, radiologists rely on seeing signs of the injury rather than the injury itself. However, since the brainstem is a common victim of this injury, many patients with atlanto-occipital dislocation will not survive to the ED.
Hangman’s fracture, or “traumatic spondylolisthesis of the axis” if you’re feeling fancy, is typically caused by a forceful hyperextension event (a short drop and a sudden stop, shoutout to any Pirates of the Caribbean fans). This results in a fracture going through both “pars interarticulari” (that portion connecting the front of the vertebrae to the back). This can cause varying degrees of subluxation of C2 on C3 from associated ligamentous injuries and resultant spinal cord injuries.
Teardrop fractures come in a couple of different flavors, namely extension and flexion. Extension teardrop occurs from forced extension (duh!) causing an avulsion of the anteroinferior corner of the vertebral body. Flexion teardrop occurs from forced flexion (also duh!) causing an avulsion of the anteroinferior corner of the vertebral body. So, how are you supposed to tell the difference, and is the difference important? Well, yes! Flexion tear drop fractures are more unstable since the interspinous ligament can be torn, while extension fractures typically involve injury to the anterior longitudinal ligament and don’t often result in spinal cord injury. There are several features associated with flexion vs extension on computed tomography, but an MRI would be able to further evaluate for ligamentous injuries.6
For more information on workup and disposition, see our study guide, “C-Spine Clearance in the ED: When to ditch the collar.” If you’re having a hard time remembering the different parts of the NEXUS criteria, I use the mnemonic NSAID: Neuro deficit, Spinal tenderness to palpation, Altered mental status, Intoxicated, Distracting injury.
References
1. Jain NB, Ayers GD, Peterson EN, Harris MB, Morse L, O’Connor KC, Garshick E. Traumatic spinal cord injury in the United States, 1993-2012. JAMA. 2015 Jun 9;313(22):2236-43. doi: 10.1001/jama.2015.6250. PMID: 26057284; PMCID: PMC4712685.
2. The National Spinal Cord Injury Statistical Center. http://www.spinalcord.uab.edu/show.asp?durki=21446 (Accessed on August 7, 2022).
3. Marek RD, Falkingham PL, Benson RBJ, Gardiner JD, Maddox TW, Bates KT. Evolutionary versatility of the avian neck. Proc Biol Sci. 2021 Mar 10;288(1946):20203150. doi: 10.1098/rspb.2020.3150. Epub 2021 Mar 3. PMID: 33653136; PMCID: PMC7934994.
4. Kanwar R, Delasobera BE, Hudson K, Frohna W. Emergency department evaluation and treatment of cervical spine injuries. Emerg Med Clin North Am. 2015 May;33(2):241-82. doi: 10.1016/j.emc.2014.12.002. Epub 2015 Mar 14. PMID: 25892721.
5. Pimentel L, Diegelmann L. Evaluation and management of acute cervical spine trauma. Emerg Med Clin North Am. 2010 Nov;28(4):719-38. doi: 10.1016/j.emc.2010.07.003. PMID: 20971389..
6. Holmes JF, Mirvis SE, Panacek EA, Hoffman JR, Mower WR, Velmahos GC; NEXUS Group. Variability in computed tomography and magnetic resonance imaging in patients with cervical spine injuries. J Trauma. 2002 Sep;53(3):524-9; discussion 530. doi: 10.1097/00005373-200209000-00021. PMID: 12352491.