Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Introduction
About 15% of HIV-infected persons in the US alone remain unaware of their infection. This leads to further morbidity later in the course of illness and increases transmission risk to others. This review will cover the diagnosis of HIV in the ED, initial symptoms of early HIV, and opportunistic infections. Post-exposure prophylaxis (PEP) is outside the scope of this review.
One of the greatest mistakes clinicians make is to rely on sexual history or IV drug abuse to guide HIV suspicion and need for testing. While asking a detailed sexual and drug use history is important, patients are reluctant to disclose this information or some may not even know their behaviors are high risk (e.g. receptive oral sex, anal intercourse, etc).
Other reasons HIV is infrequently diagnosed acutely: symptoms are nonspecific, many patients are asymptomatic, clinicians are uncomfortable asking detailed sexual and social history questions, clinicians incorrectly assume a continued validity of a previously negative HIV test.
It behooves us as clinicians to actively consider and have a low threshold to test for HIV, as some patients have had recent high-risk exposure and therefore are candidates for PEP against HIV.
Early initiation of anti-retroviral therapy (ART) reduces likelihood of HIV transmission, reduces viral reservoir, and increases the chances of HIV eradication.
HIV acquisition
By far, the greatest risk for HIV acquisition is through blood transfusion. This is virtually unheard of in the US today. Receptive anal intercourse is the 2nd most common method, followed by needle-sharing injection drug use.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Accidental needle sticks that prick the skin, mucus membrane exposure to bodily fluids (e.g. eye splash), biting, and spitting are all very low risk for HIV exposure (>1/1,000 risk).
Presentation of HIV
Acute HIV presents like any nonspecific viral syndrome, sharing many similarities with mononucleosis. In some cases, early HIV is asymptomatic in 10-60% of cases.
The usual time course from exposure to infection is about 2-4 weeks.
Classic symptoms include fever, nontender lymphadenopathy, sore throat, rash, myalgias/arthralgias, nausea/vomiting/diarrhea, weight loss, and headache.
As you can imagine, none of these symptoms are specific for HIV.
The nontender lymphadenopathy typically involves the axillary, cervical, and occipital nodes.
Sore throat is common. Painful mucocutaneous ulcers are the most distinctive finding of HIV infection.
There are shallow, sharply demarcated ulcers with white bases with surrounding erythema can be found in the mouth, anus, or penis.
Viral exanthem rash typically occurs after fever.
Aseptic meningitis rarely occurs. One study found it in ~20% of patients. Even more rare is a self-limited encephalopathy.
Pulmonary symptoms (pleuritic chest pain, productive cough) are very uncommon, and do not suggest early HIV.
Differential diagnosis: mononucleosis is perhaps the closest mimicker of HIV. It is more common and usually more recognized in teenagers. Unfortunately, HIV is often missed or not suspected.
Acute HIV is unique from other viruses in that it has mucocutaneous ulcers and a rash (both rare in mononucleosis. The only time a rash occurs in Mono is when amoxicillin is given).
Diagnosis
As stated above, even in the absence of elicited risk factors (sexual and social history), HIV could still be a possibility with the above symptoms.
Early HIV infection should be considered in those with have been recently positive for other sexually transmitted infections, regardless of their current presentation.
The most sensitive immunoassay should be performed (combination of antigen/antibody assay), plus a HIV viral load test.
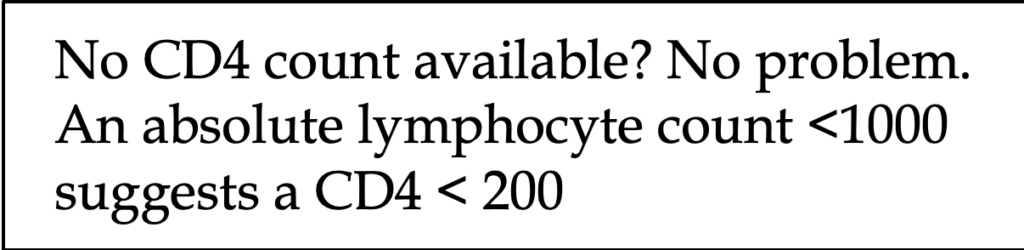
After 10-15 days of infection, viral RNA levels will typically be high, >100,000 copies/mL, and the CD4 count may drop transiently early on.
An antigen assay usually becomes positive after 15-20 days.
p24 antigen assays have greatly improved and rise with viral loads, corresponding to 30-50,000 RNA levels. Its sensitivity ranges from 90-100%. The best part is it rises around 5 days post-infection.
Following the acute course, CD4 counts rebound but never return to baseline levels.
Otherwise, labs are not helpful. Mild transaminitis, mild anemia, and thrombocytopenia have been reported but are by no means diagnostic.
It goes without saying patients should be screened for other sexually transmitted diseases.
A negative HIV screening test and negative viral load = HIV ruled out. If there is still strong suspicion, repeat testing in 1-2 weeks is very reasonable.
Negative HIV screening test and positive viral load = early HIV infection. <1000 copies/mL could mean a false positive, so repeat the test immediately.
Positive screening test and positive viral load = early or established HIV infection. Perform an antibody-only assay, if negative, then likely early HIV infection.
Opportunistic infections (OIs)
These are infections that are more frequent or more severe in patients with HIV due to immunosuppression. There are hundreds of OIs that are outside the scope of this review. Our job is to cover the most common, most classic ones.
ART is the most important strategy to prevent OIs, followed by antimicrobial prophylaxis.
The type of OI directly depends on the CD4 count as shown below:
· <500: TB, HSV, zoster, Kaposi’s
· <200: PCP (Pneumocystis jirovecii), encephalopathy, candidiasis
· <100: toxoplasmosis, histoplasmosis, cryptococcus
· <50: PML, CMV (GI, pulmonary, eye), CNS lymphoma, MIC
Pneumocystis jirovecii (formerly pneumocystis pneumonia): 50% annual risk in those with CD4 count <100.
Presentation: fever in the majority, with dry cough and progressively worsening dyspnea.
Diagnosis: CXR (bat wing appearance), showing bilateral, diffuse interstitial infiltrates. However, CXR is only abnormal in ~75%. CT chest is 100% sensitive, usually showing a ground glass pattern.
Treatment: TMP-SMX, or primaquine and clindamycin for those with sulfa allergies. Atavaquone is often quoted as an oral agent but it is for mild cases only. Pentamidine is another alternative for severe disease but can cause hypotension and hypoglycemia.
When to add steroids? A-a gradient >35 mmHg, or room air PaO2 < 70 mmHg.
Antimicrobial prophylaxis in those with CD4 counts <200: TMP-SMX
Toxoplasmosis: parasite, causes encephalitis with multifocal CNS lesions. Most common cause of focal encephalitis in AIDS.
CT head without contrast: multiple subcortical lesions. Contrast can be given which makes them appear ring-enhancing.
Treatment: Pyrimethamine plus sulfadiazine or clindamycin or azithromycin. You can also use TMP-SMX alone.
Steroids can be given if significant mass effect or edema.
Disseminated Mycobacterium avium complex (MAC): ~40% annual risk per year if CD4 count <100.
Overwhelming systemic symptoms including fever, night sweats, cough, diarrhea, weight loss.
Antimicrobial prophylaxis in those with CD4 counts <50: azithromycin
Cryptosporidium: protozoa. Causes chronic, watery diarrhea. Most common cause of chronic diarrhea in HIV patients. Fecal sample = fecal oocytes.
Treatment: supportive, start ART.
Herpes Zoster: high risk of Herpes ophthalmicus. See our podcast on Shingles and disseminated Zoster (Episode 54: Swallowing Shingles).
Cryptococcus neoformans: budding yeast, causes meningitis. From bird pigeon droppings.
Diagnosis: CT head normal. Money is in the LP. Elevated opening pressure. Classic “soap bubble” lesions and budding yeast on India ink stain, but in reality the Crypto antigen and culture are more accurate than India Ink.
Treatment: Amphotericin B plus flucytosine
Kaposi sarcoma: caused by HHV-8. Causes cutaneous, pulmonary, and GI illness (chronic diarrhea).
Cutaneous: purpura, hematomas, angiomas, nevi.
Cytomegalovirus: HHV-5. Causes esophagitis, colitis, pneumonia, and retinitis. #1 cause of blindness in HIV patients.
Presentation: visual loss, floaters.
Diagnosis of retinitis: fluffy white perivascular lesions, retinal necrosis.
Treatment: ganciclovir, foscarnet
References
1. Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Department of Health and Human Services. Available at http://aidsinfo.nih.gov/contentfiles/lvguidelines/AdultandAdolescentGL.pdf (Accessed on August 05, 2019).
2. Robb ML, Eller LA, Kibuuka H, et al. Prospective Study of Acute HIV-1 Infection in Adults in East Africa and Thailand. N Engl J Med 2016; 374:2120
3. Daar ES, Little S, Pitt J, et al. Diagnosis of primary HIV-1 infection. Los Angeles County Primary HIV Infection Recruitment Network. Ann Intern Med 2001; 134:25.
4. Gaines H, von Sydow M, Pehrson PO, Lundbegh P. Clinical picture of primary HIV infection presenting as a glandular-fever-like illness. BMJ 1988; 297:1363.
5. Schacker T, Collier AC, Hughes J, et al. Clinical and epidemiologic features of primary HIV infection. Ann Intern Med 1996; 125:257.
6. Lapins J, Gaines H, Lindbäck S, et al. Skin and mucosal characteristics of symptomatic primary HIV-1 infection. AIDS Patient Care STDS 1997; 11:67.
7. Rich JD, Merriman NA, Mylonakis E, et al. Misdiagnosis of HIV infection by HIV-1 plasma viral load testing: a case series. Ann Intern Med 1999; 130:37.
8. Cohen MS, Gay CL, Busch MP, Hecht FM. The detection of acute HIV infection. J Infect Dis 2010; 202 Suppl 2:S270.
9. Pandori MW, Hackett J Jr, Louie B, et al. Assessment of the ability of a fourth-generation immunoassay for human immunodeficiency virus (HIV) antibody and p24 antigen to detect both acute and recent HIV infections in a high-risk setting. J Clin Microbiol 2009; 47:2639.
10. Adler MW. ABC of Aids: Development of the epidemic. BMJ 2001; 322:1226.
11. Gutteridge, David L MD, MPH, Egan, Daniel J. MD. The HIV-Infected Adult Patient in The Emergency Department: The Changing Landscape of the Disease. Emergency Medicine Practice: An Evidence-Based Approach to Emergency Medicine. Vol 18, Num 2. Feb 2016.