Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Larry Mellick, MD
Introduction
A “brief resolved unexplained event” or BRUE, is not a specific diagnosis, but rather a diverse group of patients with various pathology. It reflects a general “catch-all” chief complaint. It peaks in incidence at <2 months of age but can occur anytime within the first year of life. The real challenge is to identify which infants require further investigation versus those who can be discharged from the ED. The old term was ALTE (apparent life-threatening event), but this term was too broad and incorrectly associated symptoms and SIDS. Incidence of BRUE rates are not completely known, but it is suggested to be around 3-40 per 10,000 infants.
This review will cover the risks of BRUE, common causes, along with workup and disposition.
Clinical features that define BRUE (includes any of the following):
– cyanosis or pallor
– absent, decreased, or irregular breathing
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
– change in tone
– altered mental status
Estimated duration of the event is typically <1 minute. The term BRUE can only be applied if the infant is asymptomatic on presentation in the ED. If not, another diagnosis should be sought.
Risk Factors
Risk factors include issues with feeding, maternal smoking history, premature birth or low birth weight, recent upper respiratory illness, age <2 months old, history of prior episodes, gastroesophageal reflux (GER), and seizures.
Causes are many, but the most common ones uncovered include GER, seizures, and respiratory infections which account for the vast majority of BRUEs.
Child abuse is the cause in <10% of cases.
Cardiac disease, upper airway obstruction, metabolic diseases, bacterial infections <3% of cases.
Evaluation
The most important part of BRUE evaluation is the history and physical exam, as it allows the clinician to decide on the infant being low or high risk. In fact, one study demonstrated the history/physical alone diagnosed ~20% of cases. Another 50% of diagnoses were confirmed from testing that was prompted by the history/physical.
In other words, the most critical diagnostic tool is a description of the episode, with as much detail as possible.
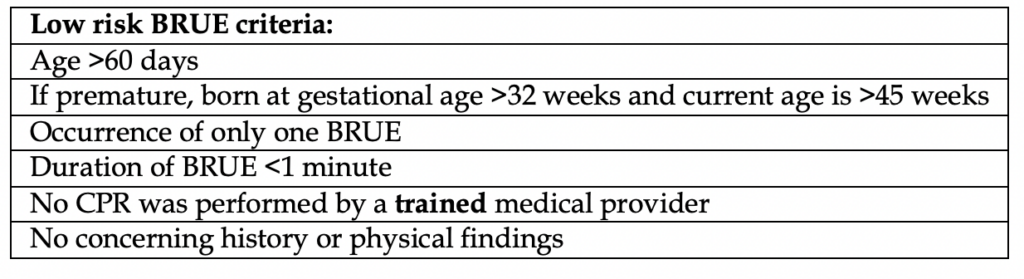
The decision to proceed with workup depends on if the presentation is deemed “high risk” or “low risk”. See table below for details:
So what are the concerning historical and physical exam findings?
In simplest terms, anything that suggests a tangible, concerning cause: Child abuse, respiratory illness, trauma, ingestion, developmental delay, congenital anomalies, or family history of sudden unexplained death in a primary relative.
Physical exam findings are fairly obvious and include injuries (e.g. bleeding/bruising), bulging fontanelle, altered status, fever, respiratory distress, decreased pulses, or abdominal distension or masses.
Infants who are low risk do not benefit from any further investigation. These patients are managed outpatient and no further intervention is required in the ED.
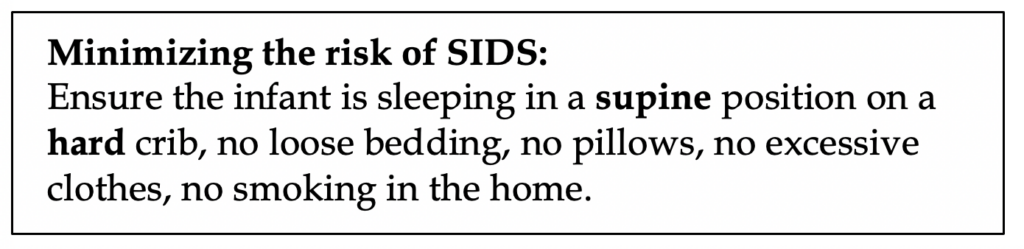
Recommended: extensive education about BRUE with caregivers, reinforce measures to prevent sudden infant death syndrome (SIDS), offer resources in CPR, and arrange f/u in 24 hours with PCP. Parents should be told never to shake the infant if unresponsive.
Not recommended by the American Academy of Pediatrics (AKA do not do): any lab work, chest x-ray, echocardiogram, or any other diagnostic tests.
Here’s a bombshell: no cardiopulmonary monitoring for these patients at home. If you are that concerned about the infant then admit them.
Optional: if you are unsure about the patient, brief ED observation for 1-4 hours is not unreasonable, a 12-lead EKG is not unreasonable either.
Lastly, if you are going to order one diagnostic test, pertussis testing is not a bad idea in those with respiratory symptoms.
High risk infants
Admit and do a full workup. Continuous cardiopulmonary monitoring, EKG, CBC, BMP, respiratory viral panel and pertussis testing are all typically performed. Further diagnostic studies are tailored to the patient based on the findings from the history and physical. Many of these tests are outside the scope of emergency medicine, as these will occur inpatient, but you still should be familiar with them as they are related to many other pathologies that present on their own to the ED.
If there are neurological findings or concern for child abuse, CT head is warranted.
RSV and pertussis are known to cause sudden infant death in premature infants, hence their routine testing.
Hypoglycemia and vomiting might suggest metabolic disease like inborn errors of metabolism.
Suggestion of seizure-activity might prompt inpatient EEG and neuroimaging.
A word on GER…
GER is a common cause of BRUE by mechanism of laryngospasm. There is no evidence that treating GER prevents future episodes.
Features that suggest GER include regurgitated food at the time of event, infant was awake, and feeding was recent or at time of event.
It is not recommended to start antihistamines or other anti reflux agents. Have them follow up with their pediatrician for further GERD discussion.
Prognosis
Recurrence risk ranges 10-25% in several studies for ALTE, with an overall death rate of <1%. There are no new studies on BRUE mortality rates at the time of this writing.
Risks for recurrence include respiratory illness, prematurity, and history of prior events.
There is no established relationship between BRUE and SIDS. SIDS occurs without warning and no studies have documents preexisting cases of apnea.
References
- Tieder JS, Bonkowsky JL, Etzel RA, et al. Clinical Practice Guideline: Brief Resolved Unexplained Events (Formerly Apparent Life-Threatening Events) and Evaluation of Lower-Risk Infants: Executive Summary. Pediatrics. 2016:137(5):e20160591.
- Colombo M, Katz ES, Bosco A, et al. Brief resolved unexplained events: Retrospective validation of diagnostic criteria and risk stratification. Pediatr Pulmonol 2019; 54:61.
- Tieder JS, Bonkowsky JL, Etzel RA, et al. Brief Resolved Unexplained Events (Formerly Apparent Life-Threatening Events) and Evaluation of Lower-Risk Infants. Pediatrics 2016; 137.
- Merritt JL 2nd, Quinonez RA, Bonkowsky JL, et al. A Framework for Evaluation of the Higher-Risk Infant After a Brief Resolved Unexplained Event. Pediatrics 2019; 144.
- Polberger S, Svenningsen NW. Early neonatal sudden infant death and near death of fullterm infants in maternity wards. Acta Paediatr Scand 1985; 74:861.
- Kiechl-Kohlendorfer U, Hof D, Peglow UP, et al. Epidemiology of apparent life threatening events. Arch Dis Child 2005; 90:297.
- Fu LY, Moon RY. Apparent life-threatening events: an update. Pediatr Rev 2012; 33:361.
- Brand DA, Altman RL, Purtill K, Edwards KS. Yield of diagnostic testing in infants who have had an apparent life-threatening event. Pediatrics 2005; 115:885.
- Kahn A, European Society for the Study and Prevention of Infant Death. Recommended clinical evaluation of infants with an apparent life-threatening event. Consensus document of the European Society for the Study and Prevention of Infant Death, 2003. Eur J Pediatr 2004; 163:108.