Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Objectives: Review CNS layers, define meningitis, causes, diagnoses, treatment, and complications
Introduction
The CNS is protected by several layersin addition to its blood brain barrier. In order: scalp à skull à dura mater (“tough mother in Latin”) à arachnoid mater à pia mater à brain parenchyma
Meningitis: inflammation of the meninges, the protective layers of the CNS (brain and spinal cord).
Two types of meningitis:
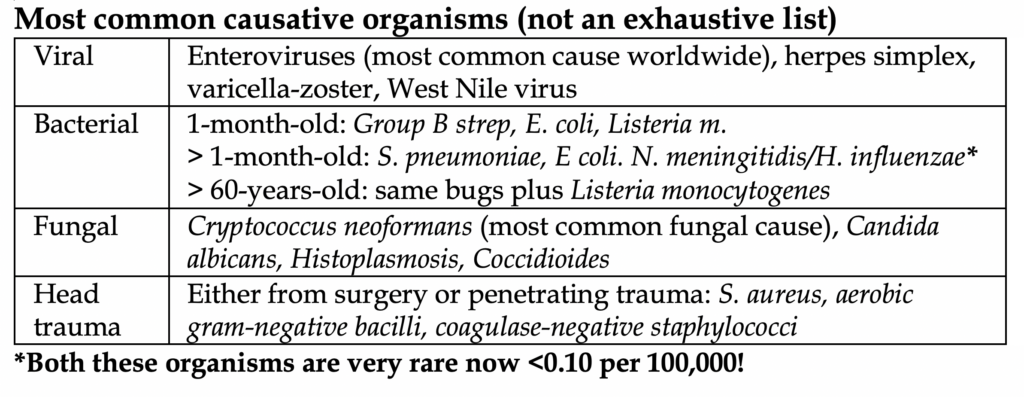
Aseptic: meningitis with negative cultures. Viral is the most common cause of meningitis overall. Rarely, aseptic meningitis can be autoimmune.
Septic: bacterial cause. Specific organisms are mentioned below. Historically, mortality was very high, now with routine immunization against Haemophilus influenzae and Neisseria Meningitidis, it has greatly reduced the frequency in children and now the disease primarily affects adults. By far, Streptococcus pneumoniae is the most common bacterial cause in developed countries.
Pathophysiology: organisms enter the meninges via two possible mechanisms.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
1) Hematogenous spread
2) Direct inoculation from prior skull trauma, nasal cavity, or indwelling skull devices.
Crossing the blood brain barrier (BBB): no easy task. Invading organisms must somehow transverse the mighty BBB, which blocks the vast majority of organisms, toxins, and certain ions from entering the CNS. Organisms can utilize 3 special methods to bypass this significant barrier:
1) Enter through the choroid plexus or other circumventricular organs (these areas lack a BBB)
2) use of capsules
3) local destruction of the endothelial cell barrier
Tools of the trade
-Capsule: helps adhesion to surfaces; prevents phagocytosis (Strep Pneumoniae, Neisseria)
-Pili: attach to surfaces and can contain toxins. (Neisseria, E. coli).
-LPS: endotoxin that induces septic shock (Neisseria).
-IgA protease: ability to cleave IgA and evade.
Why is meningitis so awful? Massive inflammation!
In septic meningitis, there is lysis of invading bacteria by local astrocytes à release of toxins and bacterial components leads to massive cytokine release which recruit other immune mediators à increased BBB permeability à cerebral edema à increased intracranial pressure à decreased perfusion of brain tissue à brain tissue ischemia
Patients can quickly progress to septic shock, they are at high risk for disseminated intravascular coagulation (DIC).
Presentation
Patients typically present within 24 hours of symptoms.
<50% actually have the classic “meningismus” triad of fever, nuchal rigidity, and change in mental status.
The most common clinical features: severe headache (84%), fever (75%), and GCS <14 (70%).
A study in 2004 found that in 696 cases of bacterial meningitis, 95% of patients had 2 of the 4: headache, stiff neck, fever, altered mental status. The absence of any of these findings virtually excludes meningitis.
Specific neurologic findings are very uncommon: seizures (~20%), aphasia or monoparesis (~20%), coma/cranial nerve palsy/papilledema/rash all <15% and therefore unreliable.
Children and teenagers often do not exhibit any of these symptoms/signs and might just appear irritable with a fever.
Older adults are more likely to have severe symptoms, especially those with Listeria meningitis.
Viral meningitis patients classically present mildly sick, often with viral syndrome symptoms and development of a headache.
N. meningitidis, despite being rare, is a very bad bug. It can cause meningococcemia in patients.
Meningococcemia: a form of DIC due to N. meningitidis.
-Diffuse purpuric rash (10-25%)
-Signs of distributive shock
-Waterhouse-Friderichsen syndrome (adrenal hemorrhage and failure)
Physical exam:
Nuchal rigidity testing: passive or active neck flexion can result in an inability to touch the chin to the chest (sensitivity 30%, specificity 70%).
Kernig Sign: when hip is flexed at 90o, reluctance to extending knee due to pain.
Brudzinski Sign: when neck is passively flexed, the patient will spontaneously flex hips.
The latter two signs make logical sense, however, in the modern era they are poorly sensitive. The signs were originally developed and tested in patients with severe, late untreated bacterial and TB meningitis in the pre-antibiotic era. In one large study the sensitivity and specificity was found to be 5% and 95%, respectively.
The classic skin manifestation of N. meningitidis is not common, 10-25%. Its description varies, and most commonly is maculopapular or petechial. It is not at all specific for Neisseria.
In summary, physical exam is not helpful early in the disease course. The history, combined with an LP, make the diagnosis.
Workup: full “septic workup”. CBC, CMP, lactate, blood cultures, early IV fluids if hypotensive. Have a low threshold to starting vasopressors. If concern for septic shock and progression to DIC, add on coagulation studies. Leukopenia, thrombocytopenia, and low fibrinogen carry a poor prognosis.
50-90% of patients with meningitis have positive blood cultures. N. meningitidis is historically difficult to speciate.
The money is in the lumbar puncture. LP is necessary to establish a diagnosis and determine the causative organism.
CT before LP? Not always.
There is a theoretical fear of herniation due to rapid change in CSF pressure from LP. The concern is the presence of some mass lesion or bleeding, thus raising ICP in the skull. The vast majority of patients have none of these, so you should only perform CT head prior to LP if any of the following are present: immunocompromised, any history of some intracranial pathology (masses, prior stroke/hemorrhage, abscess), papilledema on exam, altered mental status from baseline, neurological focal deficit, new onset seizures.
Other contraindications to LP: intracranial mass, overlying infection at lumbar site or spinal epidural abscess, thrombocytopenia <50k, INR >1.6.
Why not just CT everyone? For starters, that’s not very ethical given the level of radiation. Secondly, CT delays LP and is of no clinical benefit if none of the above indications are met.
It should be emphasized that empiric antibiotic therapy should not be delayed if there is a contraindication or inability to perform LP. Giving antimicrobials has minimal effects on the chemistry and cytology of the LP. However, there is a reduction in yield of the gram stain and culture.
Opening pressure (can only be performed in lateral decubitus position): bacterial meningitis and HSV encephalitis very often have values >200 mmHg.
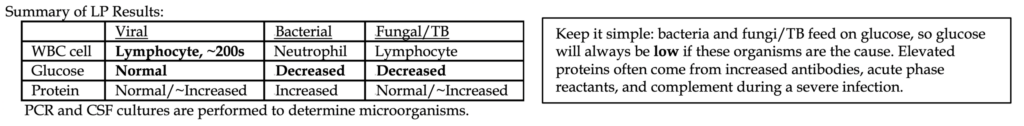
In reality, LP results are on a massive spectrum. Only ~66% have a CSF WBC >1000. Another cause of elevated WBC and RBC is a subarachnoid hemorrhage.
If a traumatic LP is suspected and RBC count is high, subtract one WBC for every 500-1000 RBCs measured in CSF. CSF lactate is also a helpful test and has been found to be more accurate than WBC/glucose/protein counts when differentiating bacterial from aseptic meningitis.
Gram stain has nearly 100% specificity, its sensitivity ranges too much to be reliable.
Treatment
Aseptic meningitis
Due to a likely viral cause, only supportive therapy is needed in those with minimal symptoms, young age, and/or lack of other comorbidities. Only close monitoring is warranted. Have suspicion for HIV and herpes in certain patients. Make sure to exclude encephalitis (patient will have altered mental status). Herpes and varicella will receive acyclovir. Other viral causes of aseptic meningitis deserve their own respective evaluations.
Septic meningitis
Neonatal regimen: Ampicillin plus cefotaxime. OR Ampicillin plus gentamicin
Childhood regimen: Vancomycin, ceftriaxone or cefotaxime
Adult regimen: Vancomycin, ceftriaxone or cefotaxime. Dexamethasone prior to antibiotics if unknown organism. Ampicillin if >65 y/o
Vancomycin (Strep and other gram-positive coverage)
Ceftriaxone (Neisseria and other gram-negative coverage)
Ampicillin (Listeria coverage)
Amphotericin B and Flucytosine (fungal coverage)
Meropenem or Moxifloxacin can be substituted for the cephalosporins if there is an anaphylactic penicillin allergy
Dexamethasone? It has been studied as an adjuvant therapy to reduce the neurological complications in adults and children. It is controversial and there’s a lot of chit-chat on this subject, but we’ll spare you and tell you what you need to know.
In general, in developed countries, the guidelines recommend giving 0.15 mg/kg dexamethasone before or at the same time as antimicrobials if there is strong suspicion for bacterial meningitis, but the organism is unknown. It should only be continued if the organism is found to be S. pneumoniae. There is no proven benefit of continuing steroids if the organism is not S. pneumoniae.
Dexamethasone should not be given after antibiotics as its benefit is very limited and there might even be an increase in mortality.
In developing countries, dexamethasone has a less clear role and no proven benefit.
In children, steroids are only indicated in those with H. influenzae B meningitis. It can reduce the risk of hearing loss. Steroids should be given prior to, or with the first dose of antibiotics and continued for 4 days. Since H. influenzae is exceedingly rare, we only give steroids in unvaccinated children with suspected meningitis.
References
1. Pfister HW, Feiden W, Einhäupl KM. Spectrum of complications during bacterial meningitis in adults. Results of a prospective clinical study. Arch Neurol 1993; 50:575.
2. de Gans J, van de Beek D, European Dexamethasone in Adulthood Bacterial Meningitis Study Investigators. Dexamethasone in adults with bacterial meningitis. N Engl J Med 2002; 347:1549.
3. Scarborough M, Gordon SB, Whitty CJ, et al. Corticosteroids for bacterial meningitis in adults in sub-Saharan Africa. N Engl J Med 2007; 357:2441.
4. Brouwer MC, McIntyre P, Prasad K, van de Beek D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst Rev 2015; :CD004405.
5. Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 2004; 39:1267.
6. van de Beek D, de Gans J, Spanjaard L, et al. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med 2004; 351:1849.
7. Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 2004; 39:1267.
8. van de Beek D, Cabellos C, Dzupova O, et al. ESCMID guideline: diagnosis and treatment of acute bacterial meningitis. Clin Microbiol Infect 2016; 22 Suppl 3:S37.
9. McGill F, Heyderman RS, Michael BD, et al. The UK joint specialist societies guideline on the diagnosis and management of acute meningitis and meningococcal sepsis in immunocompetent adults. J Infect 2016; 72:405.
10. Castelblanco RL, Lee M, Hasbun R. Epidemiology of bacterial meningitis in the USA from 1997 to 2010: a population-based observational study. Lancet Infect Dis 2014; 14:813.
11. Vallejo JG, McNeil JC, Hultén KG, et al. Invasive Haemophilus influenzae Disease at Texas Children’s Hospital, 2011 to 2018. Pediatr Infect Dis J 2019; 38:900.
12. Bijlsma MW, Brouwer MC, Kasanmoentalib ES, et al. Community-acquired bacterial meningitis in adults in the Netherlands, 2006-14: a prospective cohort study. Lancet Infect Dis 2016; 16:339.
13. van de Beek D, de Gans J, Spanjaard L, et al. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med 2004; 351:1849.
14. Weisfelt M, van de Beek D, Spanjaard L, et al. Community-acquired bacterial meningitis in older people. J Am Geriatr Soc 2006; 54:1500.
15. Aronin SI, Peduzzi P, Quagliarello VJ. Community-acquired bacterial meningitis: risk stratification for adverse clinical outcome and effect of antibiotic timing. Ann Intern Med 1998; 129:862.
16. Attia J, Hatala R, Cook DJ, Wong JG. The rational clinical examination. Does this adult patient have acute meningitis? JAMA 1999; 282:175.
17. Durand ML, Calderwood SB, Weber DJ, et al. Acute bacterial meningitis in adults. A review of 493 episodes. N Engl J Med 1993; 328:21.
18. Thomas KE, Hasbun R, Jekel J, Quagliarello VJ. The diagnostic accuracy of Kernig’s sign, Brudzinski’s sign, and nuchal rigidity in adults with suspected meningitis. Clin Infect Dis 2002; 35:46.
19. Thomas AE, Baird SF, Anderson J. Purpuric and petechial rashes in adults and children: initial assessment. BMJ 2016; 352:i1285.
20. Kaplan SL. Clinical presentations, diagnosis, and prognostic factors of bacterial meningitis. Infect Dis Clin North Am 1999; 13:579.
21. Rogers T, Sok K, Erickson T, et al. Impact of Antibiotic Therapy in the Microbiological Yield of Healthcare-Associated Ventriculitis and Meningitis. Open Forum Infect Dis 2019; 6:ofz050.
22. Hasbun R, Abrahams J, Jekel J, Quagliarello VJ. Computed tomography of the head before lumbar puncture in adults with suspected meningitis. N Engl J Med 2001; 345:1727.
23. Gopal AK, Whitehouse JD, Simel DL, Corey GR. Cranial computed tomography before lumbar puncture: a prospective clinical evaluation. Arch Intern Med 1999; 159:2681.
24. Tunkel AR, Hartman BJ, Kaplan SL, et al. Practice guidelines for the management of bacterial meningitis. Clin Infect Dis 2004; 39:1267.
25. Salazar L, Hasbun R. Cranial Imaging Before Lumbar Puncture in Adults With Community-Acquired Meningitis: Clinical Utility and Adherence to the Infectious Diseases Society of America Guidelines. Clin Infect Dis 2017; 64:1657.



