Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Monica Mitta, MS4
Peer editor: Blake Briggs, MD, Travis Smith DO, Mary Claire O’Brien, MD
Objectives: explain the pathophysiology and common exam findings in patients with pneumothorax; interpret imaging findings associated with pneumothorax; and discuss appropriate treatment options and disposition.
Introduction
It’s hard to criticize Harry Potter. After all, he saves the world from the evil He-Who-Must-Not-Be-Named. However, did you know that Harry Potter nearly killed someone with a pneumothorax? When Aunt Marge begins insulting his parents, Harry unintentionally casts an inflating charm, causing her to blow up like a balloon. The increased pressure in her pleural cavity would have likely collapsed her lungs and compromised nearby structures. Luckily, the Ministry of Magic punctures her in time and ultimately prevents cardiovascular collapse.
A pneumothorax (PTX) is any air in the pleural space. It occurs when air fills the pleural space, causing partial or full collapse of the lungs. Air can enter this space through communication with lung parenchyma or the outside environment.
Overall, there are two types of PTX: spontaneous and traumatic. Trauma is the most common cause of pneumothorax.
Primary spontaneous PTX: no underlying clinical lung disease, no external cause (subpleural bleb rupture or bullous rupture). It is unknown how subpleural blebs form, but they are more common in tall, thin males 10-30 years old. Primary spontaneous PTX is up to 6x more common in men, with a rate of 7.4 per 100,000 people in the US alone. The biggest risk factor is smoking. Depending on daily cigarette use, the risk in smokers vs. nonsmokers is a difference of 12% vs 0.1%, respectively.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Secondary spontaneous PTX: a complication of some underlying disease. Typically seen in older patients >55 years old. COPD is the most common risk factor, implicated in 50-70% of cases. Other conditions include ILD, Marfan syndrome, Ehlers-Danlos, alpha-1 antitrypsin deficiency, malignancy, CF, TB, and sarcoidosis.
Despite most patients with primary PTX having “no known disease,” most have some sort of unrecognized disease like subpleural blebs, bullae, or other inherited conditions, changing the distinction of primary to secondary. In reality, this is all likely on some sort of spectrum.
Traumatic PTX: also known as acquired PTX, arises from iatrogenic or some form of blunt or penetrating trauma.
Open traumatic PTX: caused by penetrating trauma, air enters from exterior
Closed traumatic PTX: caused by blunt trauma, air enters from hole in lung
Tension PTX: “one-way valve” phenomenon allows air into the pleural space, but not back out. The increasing pressure can collapse nearby mediastinal structures. Venous return to the heart decreases, leading to obstructive shock. More on that below.
Clinical Presentation
PTX should be on the differential for any patient presenting with acute dyspnea or chest pain. Symptoms can present either suddenly or be gradual in onset. Chest pain is often sharp, pleuritic, and unilateral. Less commonly, pain can predominate in the shoulders or back. Dyspnea may often worsen progressively as the PTX expands. Less common symptoms include cough, fever, anxiety, fatigue, and upper abdominal pain. Complications of PTX include hemorrhage, empyema, effusions, pneumomediastinum, and dysrhythmias.
Symptoms are related to the volume of air present in the PTX, but amazingly there are cases of otherwise healthy, young patients walking into triage with dyspnea and complete collapse of a lung, saturating >95% on room air. A high index of suspicion is warranted, and one should not rely on the history alone.
Vital sign abnormalities are key when assessing the severity of a PTX. Look for respiratory distress. Tachycardia and tachypnea can be seen early during a PTX, especially large ones. Sinus tachycardia is the most common early finding. See the table below for criteria for “unstable” patients (i.e. those with tension PTX).
The physical exam is extremely unreliable as evidence has shown that the absence of breath sounds is provider dependent. Other classic but poorly sensitive findings include hyper-resonance to percussion on the affected side, subcutaneous emphysema, as well as decreased or asymmetric chest expansion.
Tension PTX can present with cyanosis, elevated JVD and tracheal deviation to the contralateral side. More on that below.
Diagnosis
EKG and lab studies are not useful in the diagnosis of PTX, but in the undifferentiated patient, they might be warranted.
Upright chest x-ray is the traditional first step in diagnosis, but the sensitivity of chest radiographs for the detection of PTX varies between 28% and 75%. In a standard upright view, air collects in the apical regions, where a PTX is most commonly seen. A PTX is found by demonstrating a white, visceral pleural line. Look for a lack of bronchovascular markings beyond this line. Only ~50 mL of air is needed to detect a PTX in the upright x-ray. Don’t let the first rib or clavicle distract when you examine the pleural line.
Bullae can mimic PTX, but there will be a medial border appreciated concave to the chest wall. Often no white visceral pleural line is found. Do not insert chest tubes into bullae, as this can cause a PTX and increase the risk of a bronchopulmonary fistula.
Supine x-ray is not recommended as it is easier to miss a PTX. In intubated patients who require supine imaging, you may see a “deep sulcus” sign, where gas outlines the costophrenic sulcus. If any doubt, consider attempting an upright x-ray or CT.
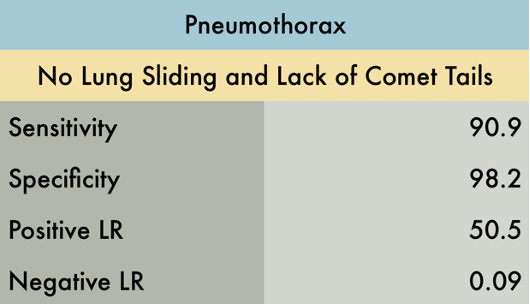
The role of ultrasound in the detection of PTX is increasing. In a study performed on patients with blunt trauma, the sensitivity and specificity of ultrasound for the detection of PTX is at least 86% and 97%, respectively. It is useful when a rapid assessment is required. It is much more sensitive than x-ray. Look for a lung sliding, comet tails (ants marching), and a lung point (marks the edge of normal pleura to PTX). The presence of a lung sliding and comet tail sign essentially excludes a PTX.
CT scan is the gold standard for diagnosis of PTX. Tells us location, size, and loculations. An occult PTX detected on CT is unlikely to produce clinical symptoms and is treated with observation if noted on imaging. CT is indicated when there is doubt about PTX vs. bullae, cavitary lesions, hydro/hemothorax with possible PTX, or other complicated cases where the diagnosis of PTX is in doubt.
Tension PTX on x-ray may demonstrate tracheal deviation to the opposite side. However, radiograph findings can also be absent. Of note, tension PTX is rare in patients with primary PTX. “Tension” occurs when air in the pleural space builds up enough pressure to interfere with venous return. This is usually due to a “one way valve” issue, where gas enters the pleural space but cannot leave during expiration. More gas increases pleural pressure and compresses the SVC, reducing venous return and eventually cardiac output.
Tension PTX is a clinical diagnosis: look for tachycardia, hypotension, tachypnea, JVD, and changes in mental status. Traditionally, it has been taught that contralateral shift of the trachea to the unaffected side and flattening of the diaphragm are evidence of tension, but this is untrue. Radiograph findings for tension might be completely absent.
Treatment and Disposition
Treatment options include either a tube thoracostomy, needle aspiration, pigtail catheter, or observation. These options are chosen based on the size of the PTX and the presence of other pathologies. Pigtail catheter placement has been increasingly utilized due to the benefits of shorter hospital stays and fewer complications, but this procedure is limited to shops with dedicated expertise. Without going into much further detail, certain specific conditions that cause secondary PTX to warrant their own specific treatments.
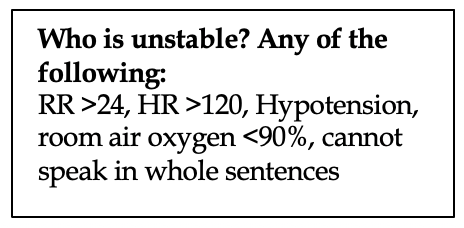
Any unstable patient is considered to have tension PTX until proven otherwise. These require rapid decompression. Stat needle decompression is immediately indicated with a large-bore (preferably 14g) inserted into the 2nd-3rdintercostal space at the midclavicular line, or the 4th-5th intercostal space at the anterior axillary line. This is always the right answer on tests, and in practice, but if an experienced provider can rapidly place a chest tube fast enough, then needle decompression is typically not needed.
Small initial spontaneous PTX (<3 cm at apex or <2 cm hilum)/primary: Observation with supplemental oxygen is first line therapy. Normal lung reabsorption is ~1-2% of pleura per day. Low flow oxygen by nasal cannula with >6mL of flow increases pleural reabsorption up to 6-fold! High flow nasal cannula or NIPPV should not be used as this can worsen the PTX. The patient can be observed for 4-6 hours, and a repeat CXR can be performed. If no abnormalities are evident and symptoms have improved, discharge home with outpatient follow up. . If not, a pigtail catheter or larger tube thoracostomy can be used as these patients have a higher likelihood of deterioration and recurrence. For those requiring oxygen, admission is warranted with CXR 12-48 hours later. Any worsening of PTX warrants a tube thoracostomy or pigtail placement. If resolution occurs, outpatient follow up in 2-4 weeks.
Large initial spontaneous PTX (>3 cm at apex or >2 cm at hilum)/secondary: options include catheter aspiration or tube thoracostomy. The decision depends on the expertise at your shop and the severity of symptoms. Interventional radiology can also be of help at many institutions. Aspiration has similar recurrence rates compared to thoracostomy; however, the initial failure rate is higher (~33%). Some providers choose thoracostomy over aspiration when patients have bilateral PTXs, complex PTX such as with loculations, or there are severe symptoms.
Tube or catheter thoracostomy: patients who fail observation or aspiration, those who are unstable, or those with recurrent presentation for primary spontaneous PTX need thoracostomy with water seal. Success rate is similar in both groups.
Chest tube thoracostomy = standard chest tube placement. In most patients, a small bore <22 Fr is optimal.
Catheter thoracostomy = <14 Fr flexible tube is placed. Unless there is blood, fluid, or empyema present, we recommend catheter thoracostomy for all patients with a PTX. Water seal is all that is required if only air is being evacuated. If the lungs fail to expand, there is worsening clinical symptoms, or an air leak develops, low wall suction at -10 cm H2O can be applied.
Consultation with CT surgery, pulmonology, or general surgery is usually indicated in those following a thoracostomy.
Summary of treatment and disposition plans
Many patients with a small primary PTX can be managed with oxygen, pain medication, and observation with repeat chest x-rays.
A larger primary spontaneous PTX or any secondary PTX will often need admission and drainage. Needle aspiration is just as effective as tube thoracostomy for the management of primary spontaneous PTX but carries the benefit of a shorter length in-hospital stay.
Patients with secondary spontaneous PTX are more likely to have persistent air leaks; thus, tube thoracostomy will often be necessary.
References
1. Brown SG, Ball EL, Perrin K, et al. Conservative versus interventional treatment for spontaneous pneumothorax. N Engl J Med 2020; 382:405-415.
2. Wilkerson RG, Stone MB. Sensitivity of bedside ultrasound and supine anteroposterior chest radiographs for the identification of pneumothorax after blunt trauma. Academic Emergency Medicine Journal 2010; 17(1):11-17.
3. Brandler ES, Fontenette D, Stone MB. Needle aspiration of spontaneous pneumothorax. Academic Emergency Medicine Journal 2010; 17(4):25-26.
4. Roberts DJ, Leigh-Smith S, Faris, PD, et al. Clinical presentation of patients with tension pneumothorax: a systematic review. Annals of Surgery 2015; 261(6):1068-1078
5. Noppen M. Spontaneous pneumothorax: epidemiology, pathophysiology and cause. European Respiratory Review 2010; 19:217-219.
6. Kattea MO, Lababede O. Differentiating pneumothorax from the common radiographic skinfold artifact. Annals of the American Thoracic Society 2015; 12(6):928-931.
7. Chiles C, Ravin CE. Radiographic recognition of pneumothorax in the intensive care unit. Crit Care Med 1986; 14:677–680.
8. Li Z, Huang H, Li Q, et al. Pneumothorax: observation. J Thoracic Disease 2014; 6(4):421-426.
9. Sharma A, Jindal P. Principles of diagnosis and management of traumatic pneumothorax. Journal of Emergencies, Trauma, and Shock 2007; 1(1):34-41.
10. Kahn HS, Wadood A, Ayyaz M. Occult pneumothorax: what do we need to do? J Coll Physicians Surg Pak 2018; 28(3):31-32.
11. Zehtabchi S, Rios CL. Management of emergency department patients with primary spontaneous pneumothorax: needle aspiration or tube thoracostomy? Annals of Emergency Medicine 2008; 51(1):91-100.
12. Ozalp A, Sevdi MS, Demirgan S, et al. Pneumothorax in the intensive care unit: retrospective analysis of two years’ experience. Bagcilar Medical Bulletin 2019; 5(1).
13. Tintinalli, JE, Stapczynskin JS, Ma OJ, et al. Tintinalli’s emergency medicine: A comprehensive study guide. Eighth edition. New York: McGraw-Hill Education, 2016.
14. Sajadi-Ernazarova KR, Martin J, Gupta N. Acute Pneumothorax Evaluation and Treatment. [Updated 2020 Aug 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from:https://www.ncbi.nlm.nih.gov/books/NBK538316/
15. The NNT. “POCUS Atlas: Pneumothorax”. https://www.thennt.com/lr/pocus-atlas-pneumothorax/



