Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Check out our free, totally awesome AIRWAY MODULE. It has live videos and amazing real life intubation breakdowns.
Author: Blake Briggs
Peer Reviewer: Mary Claire O’Brien
RSI: Quick administration of sedative and paralytic to achieve fast endotracheal intubation.
Why do we do it? One or more of the following:
1) patient’s inability to ventilate (hypercapnic respiratory failure)
2) inability to oxygenate (hypoxic respiratory failure)
3) inability to protect their own airway
4) for optimal control of the patient (i.e. to deliver care in which the patient would not tolerate or be uncooperative)
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Goal: The point is to maximize chances of success on first attempt. In RSI we must assume the stomach has contents and therefore time must be minimized till endotracheal intubation due to risks of respiratory failure and loss of airway protection, as well as aspiration from prolonged BVM. Risks of aspiration, hypotension, esophageal intubation increase with number of attempts (also 15% à50% increase in adverse events!).
Contraindications: all relative. Most important CI is difficult airway anticipation, of which rescue oxygenation is considered to be impossible or hard to achieve.
If an anatomically difficult airway is anticipated, potential for rapid desaturation, or severe hemodynamic compromise, awake intubation might be needed.
-Pros of awake intubation: avoids hemodynamic collapse, patient maintains spontaneous ventilation
-Cons: takes time, secretion control
When to delay RSI: There are key differences between “emergent” and “urgent” RSI. ABC’s is never 100% the correct order. Sometimes it needs to be BAC or CAB. Some examples:
• Patient is apneic and unresponsive. This patient needs a definitive airway immediately = ABC
• Patient is in V tach and unresponsive. Still breathing spontaneously = CAB
• Patient is not responding and has no breath sounds on right side and is hypotensive = BAC
• Patient is in shock with BP 90/50 systolic = CAB
Steps to successful RSI- 6P’s of RSI: Prepare, Preoxygenate, Positioning, Paralysis, Proof of placement, Post-intubation management
–Preparation: large bore wall suction, O2, tube, back-up plan x3, 2 large bore IVs
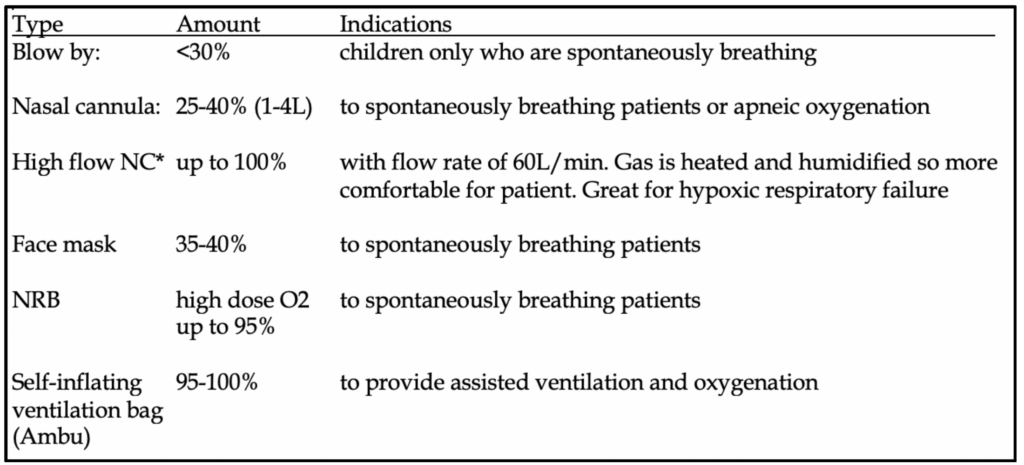
–Preoxygenate: high flow rate for minimum of 3 minutes. Replaces mixed gases in the base of lung with oxygen-rich gas for optimal FRC reservoir. 70 kg adult can maintain O2 saturation >90% for 8 minutes during apnea. Children = 4 minutes. Obesity = 3 minutes. Use bag mask for oxygen administration but no need to squeeze bag if patient is cooperative and has adequate spontaneous ventilation. Maintain nasal cannula flow during apneic period. For the very sick:
-if not able to spontaneously ventilate: positive pressure ventilation with BVM and oxygen flow at max (15 L). Try to synchronize with patient’s respiratory cycle. Do not ventilate >20 cm H2O due to risk of gastric insufflation.
-if not cooperative, NRB is used with flush oxygen.
Positioning: sniffing position with alignment of vertical axes. Jaw thrust forward and upward, patient’s head more anterior with slight upward extension.
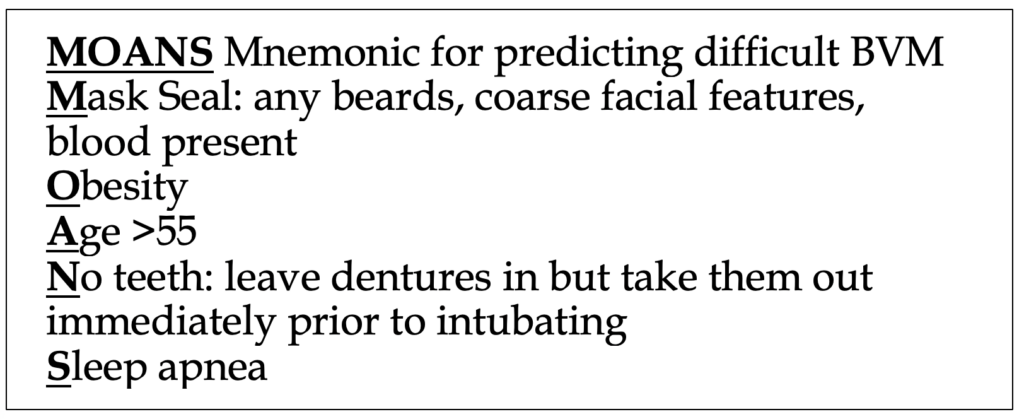
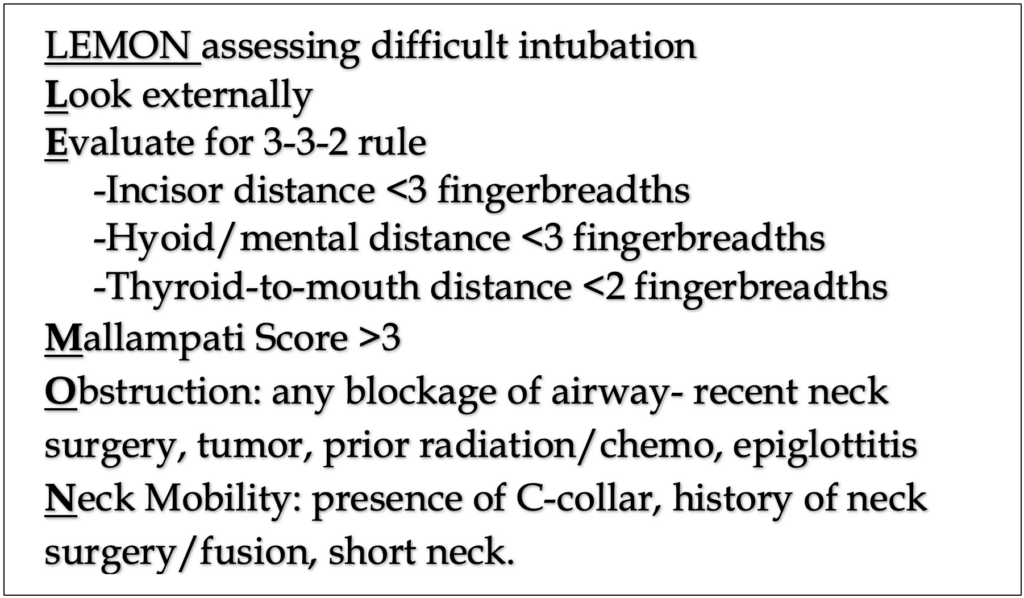
-Pre-intubation optimization: recognize and address obvious or potential pathologies and problems before RSI (see LEMON, MOANS below)Most common issue is hypotension. Causes are multifactorial and include pre-intubation drugs, bleeding, dehydration, patient’s clinical condition (e.g. shock). Must consider giving IV fluids and/or vasopressors if significant concern.
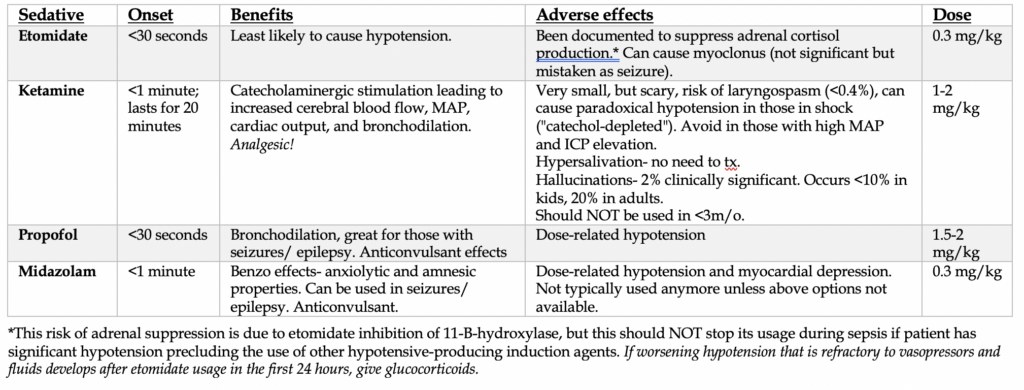
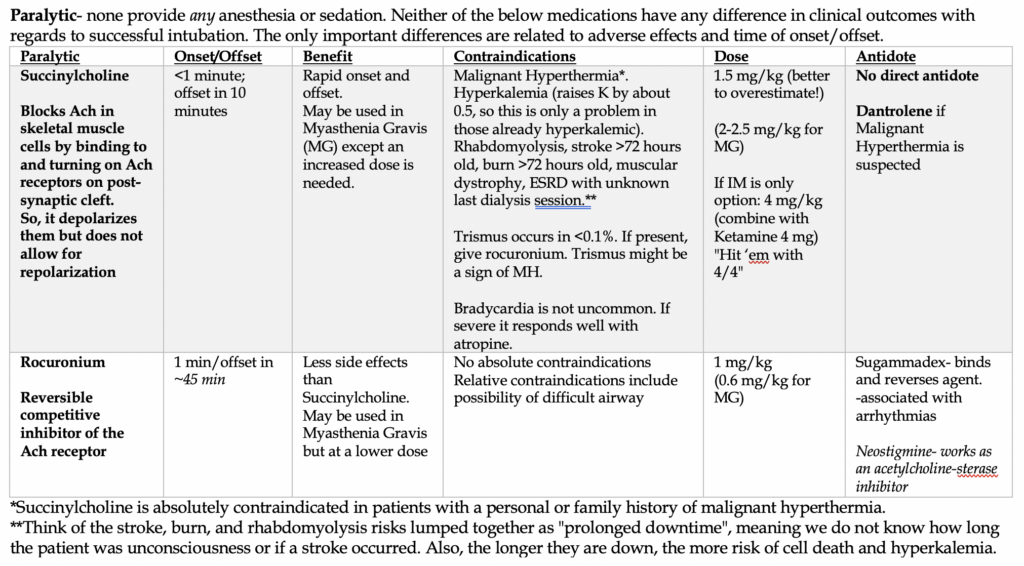
–Paralysis with induction: in the ideal situation, 2 drugs are needed for RSI: a sedative and a paralytic. Both are virtually given within 1 minute apart, with the sedative given first. All the induction agents below work as allosteric agonists of the GABA pathway in the brain. Ketamine is the exception and is primarily an NMDA antagonist.
–Placement with proof: There are many steps to ensure adequate tube placement- 1) direct glottis visualization with ETT passing through, 2) ETCO2 via monitor and color change on color-change capnographer. The CXR and listening for breath sounds as well as gastric insufflation is NOT reliable alone but should be done after color change capnography. BELIEVE the End-Tidal! It is more reliable and faster to respond to changes than Pulse Ox (this lags behind by several seconds up to 1 minute in some cases).
–Postintubation management: 1) secure the tube, 2) CXR to confirm tube positioning, 3) address any lingering preintubation problems (hypotension, shock, etc), 4) optimize the patient’s respiratory status via ventilator settings, 5) address sedation/analgesia as needed.
What if hypotension does not improve after initial recovery from apnea? Think about pneumothorax, tracheal tube cuff rupture, mucus plugging, esophageal intubation.
References
1. Li J, Murphy-Lavoie H, Bugas C, et al. Complications of emergency intubation with and without paralysis. Am J Emerg Med 1999; 17:141.
2. Cicala R, Westbrook L. An alternative method of paralysis for rapid-sequence induction. Anesthesiology 1988; 69:983.
3. Bozeman WP, Kleiner DM, Huggett V. A comparison of rapid-sequence intubation and etomidate-only intubation in the prehospital air medical setting. Prehosp Emerg Care 2006; 10:8.
4. Lundstrøm LH, Duez CH, Nørskov AK, et al. Avoidance versus use of neuromuscular blocking agents for improving conditions during tracheal intubation or direct laryngoscopy in adults and adolescents. Cochrane Database Syst Rev 2017; 5:CD009237.
5. Topulos GP, Lansing RW, Banzett RB. The experience of complete neuromuscular blockade in awake humans. J Clin Anesth 1993; 5:369.
6. Naguib M, Samarkandi AH, El-Din ME, et al. The dose of succinylcholine required for excellent endotracheal intubating conditions. Anesth Analg 2006; 102:151.
7. Lemmens HJ, Brodsky JB. The dose of succinylcholine in morbid obesity. Anesth Analg 2006; 102:438.
8. Levitan R. Safety of succinylcholine in myasthenia gravis. Ann Emerg Med 2005; 45:225.
9. Gronert GA. Cardiac arrest after succinylcholine: mortality greater with rhabdomyolysis than receptor upregulation. Anesthesiology 2001; 94:523.
10. Martyn JA, Richtsfeld M. Succinylcholine-induced hyperkalemia in acquired pathologic states: etiologic factors and molecular mechanisms. Anesthesiology 2006; 104:158.
11. Magee DA, Gallagher EG. “Self-taming” of suxamethonium and serum potassium concentration. Br J Anaesth 1984; 56:977.
12. Carroll JB. Increased incidence of masseter spasm in children with strabismus anesthetized with halothane and succinylcholine. Anesthesiology 1987; 67:559.
13. Sims C. Masseter spasm after suxamethonium in children. Br J Hosp Med 1992; 47:139.
14. Perry JJ, Lee J, Wells G. Are intubation conditions using rocuronium equivalent to those using succinylcholine? Acad Emerg Med 2002; 9:813.
15. Nava-Ocampo AA, Velázquez-Armenta Y, Moyao-García D, Salmerón J. Meta-analysis of the differences in the time to onset of action between rocuronium and vecuronium. Clin Exp Pharmacol Physiol 2006; 33:125.
16. Blichfeldt-Lauridsen L, Hansen BD. Anesthesia and myasthenia gravis. Acta Anaesthesiol Scand 2012; 56:17.



