Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Burch, PharmD, OMS IV
Peer editors: Travis Smith, DO, Blake Briggs, MD, Mary Claire O’Brien, MD
Introduction
Acetylcholine is a familiar neurotransmitter with many different roles. Anticholinergics are substances that antagonize the actions of the neurotransmitter acetylcholine at the muscarinic receptors. More than 600 compounds with anticholinergic activity have been identified, and there were nearly 14,000 exposures to these substances in 2015.1 Anticholinergic can be employed for a variety of different medical conditions, including urinary incontinence, chronic obstructive pulmonary disease, motion sickness, cholinergic toxicity, and Parkinson’s disease, just to name a few.2 Anticholinergic toxicity is encountered relatively frequently in the emergency department, so it is important that emergency providers promptly and efficiently recognize the toxidrome. This review will cover the pathophysiology, presentation, and management of anticholinergic toxicity. Children and adults have very similar presentations and management, with the only difference being that in children the most common cause is unintentional ingestions. Teenagers and young adults may ingest certain compounds for hallucinogenic properties (like jimson weed) or suicide.3
Pathophysiology
Muscarinic receptors are present on the target organ cells of the parasympathetic nervous system and sweat glands in the sympathetic nervous system. In an overdose, anticholinergics antagonize muscarinic receptors, which can lead to the following clinical manifestations 2:
– General: hyperthermia 4
– Cardiovascular: tachycardia, flushing, and dysrhythmias 4,5
– Gastrointestinal: decreased gut motility, constipation, vomiting, decreased saliva and tear production
– Genitourinary: urinary retention 4,6
– HEENT: blurry vision, mydriasis, narrow-angle glaucoma, potential vision loss4
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
– Skin: Dry skin through the inhibition of sweating 7
– Musculoskeletal: diminished muscle contraction
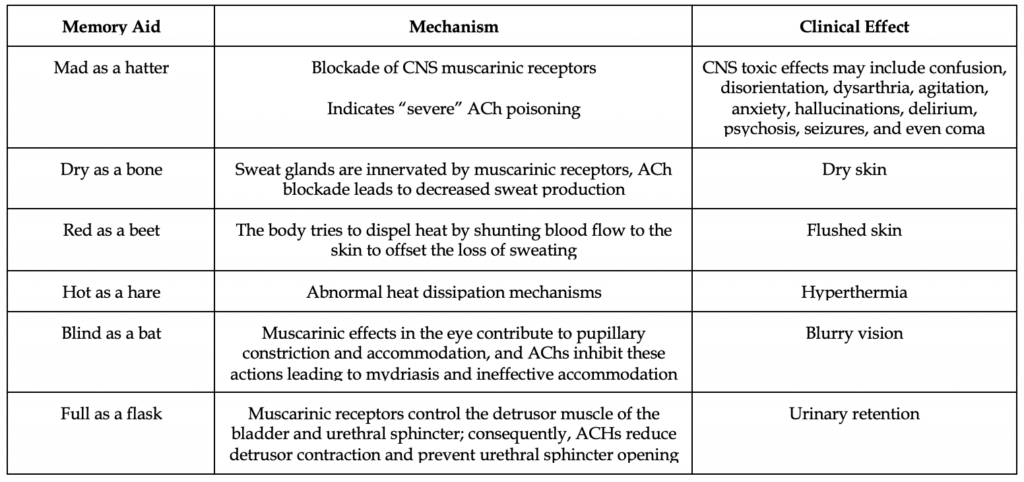
The useful memory aid “red as a beet, dry as a bone, blind as a bat, mad as a hatter, hot as a hare, and full as a flask” helps to remember the common signs and symptoms of anticholinergic toxicity. The adverse effects of anticholinergics can be divided into central and peripheral effects.
Central effects result from excess blockade of muscarinic receptors within the CNS. Peripheral adverse effects result from the antagonism of exocrine glandular secretion, muscle contraction, and end-organ targets of the peripheral parasympathetic nervous system.4 The onset of anticholinergic toxicity varies depending on the toxin but typically begins within one to two hours of oral ingestion.
Presentation
Anticholinergic toxicity is characterized as peripheral, central, or both. While peripheral signs alone are less concerning, the presence of central findings is consistent with a moresevereclinical picture. Central effects often develop together with peripheral effects but may persist longer or appear after peripheral effects resolve. Patients with central CNS toxicity require longer observation and more aggressive care. Decreased or absent bowel sounds and tachycardia are the first indications of acute anticholinergic toxicity.4
In addition, you need to recognize chronic anticholinergic toxicity. Patients treated with multiple medications that possess anticholinergic effects may present with more elusive symptoms consistent with anticholinergic toxicity, like altered mental status. These patients may not present with all the traditional signs and symptoms of anticholinergic toxicity, and their presentation may be wrongly attributed to a different diagnosis. It is important for you to be aware of the classes of medications with anticholinergic properties.
Diagnosis
Anticholinergic poisoning should be considered in all patients presenting with an altered mental status and physical exam findings consistent with anticholinergic toxicity. The diagnosis of anticholinergic toxicity is principally based on the physical exam and common clinical manifestations. Serum drug levels of anticholinergics are not typically available and do not result in a reasonable amount of time to help with diagnosis.8
As usual, a general toxicologic workup should occur in the ED, which includes asking EMS or family members about other home medications, as well as other prescription medications found in the household. Make sure to ask about the following: specific agent, amount ingested, time of ingestion, and any potential co-ingestion. Law enforcement may need to be utilized to go to the patient’s place of residence to acquire the medication bottles if the patient is incapacitated or not being straightforward. Calling the patient’s pharmacy or any helpful EMR retrieving tricks may be beneficial.
Don’t just order the “tox workup,” as your attending might drop dead on the spot. On a basic level, some common toxicologic tests to order include salicylate and acetaminophen levels, fingerstick glucose, a CBC, a CMP to evaluate liver function, pregnancy test in women of childbearing age. Obtain an EKG to look forprolonged QRS interval, prolonged QTc interval, and possible arrhythmia. A serum creatine kinase may be ordered if rhabdomyolysis is suspected (e.g. patients with psychomotor symptoms or seizures). Doxylamine, an over-the-counter antihistamine sleep aid, has been associated with rhabdomyolysis.9
Any chemical compound or medical condition that yields a seizure, tachycardia, urinary retention, or an alteration in mental status should be included in the differential diagnosis. Many medications and diseases can cause agitated delirium. Infection should always be considered, such as meningitis, encephalitis, or sepsis. The onset of altered mental status may help. Delirium from anticholinergic toxicity usually has a more sudden onset compared to other causes. Sympathomimetic toxicity, salicylate overdose, and serotonin syndrome all cause tachycardia and hyperthermia, but only Ach toxicity has an absence of diaphoresis.
Decontamination
The majority of anticholinergic toxicity is from oral ingestion, with a minority from cutaneous and ocular absorption.10 Depending on the route and timing of exposure, GI decontamination may be performed with activated charcoal. If the patient’s mental status is intact and ingestion of an anticholinergic agent is likely, 1g/kg (maximum of 50 g) of activated charcoal should be given. Patients who refuse to swallow charcoal or cannot tolerate its administration should not be intubated solely for the purpose of charcoal administration. External decontamination may be required for topical agents.
Management
Management of any poisoned patient begins with stabilization of the airway, breathing, and circulation. Cardiac monitoring and pulse oximetry should be continued until cardiac and CNS symptoms completely resolve. A medical toxicologist should be involved as patients have better outcomes.
Sinus tachycardia is common, but typically resolves on its own. Do not jump to giving beta-blockers or other rate-altering agents. Prolonged QRS intervals and wide complex tachyarrhythmias may occur. Sodium bicarbonate has a role here, and much like TCA overdoses, can improve EKG findings and cardiotoxicity. See our handout on TCA overdose for more information on sodium bicarbonate therapy here.11
Remember to not forget about the patient’s bladder! Use POCUS to look for urinary retention, and intermittent versus indwelling catheterization might be required to relieve urinary retention.
Agitation and seizures should be treated with benzodiazepines (lorazepam 1 to 2 mg IV [pediatric dose: 0.1 mg/kg up to 2 mg maximum single dose]). Phenothiazines and butyrophenones are anticholinergic themselves. They should be avoided in most toxidrome syndromes. They are the wrong answers on test questions and clinical practice. Hyperthermia may be treated with evaporative cooling methods as needed.
Supportive care is adequate for the majority of cases. However, physostigmine should be considered in patients with moderate to severe delirium.Physostigmine is an acetylcholinesterase inhibitor that reversibly inhibits the enzyme acetylcholinesterase in both the CNS and peripheral nervous system.12 This increases the concentration of acetylcholine at the muscarinic receptors to overcome the anticholinergic blockade. Physostigmine is controversial, as cholinergic toxicity occurs if the patient does not actually have anticholinergic toxicity or if the drug is inappropriately given.13 Two retrospective studies and one randomized trial in children suggest that the management of known or suspected isolated anticholinergic poisoning with physostigmine appears to be safe with few complications.14
In short, talking with a toxicologist or poison center is highly recommended prior to administration. Atropine and resuscitative equipment should be available at the bedside and given if there are any signs of cholinergic symptoms. The adult dose is 0.5 to 2 mg (0.02 mg/kg IV up to a max of 0.5 mg per dose in pediatric patients) given via slow IV push over 5 minutes. Additionally, smaller doses may be repeated after 20 to 30 minutes if agitated delirium occurs. Physostigmine should NEVER be given if a condition other than purely anticholinergic poisoning is suspected (such as a tricyclic antidepressant overdose, see our handout on that here).
Disposition
Asymptomatic patients presenting with recent ingestion of an anticholinergic substance should receive GI decontamination with activated charcoal and should be observed in the emergency room for at least 6 hours. If the patient remains asymptomatic, they can be discharged. Patients with mild anticholinergic toxicity should be treated with activated charcoal and benzodiazepines if needed and observed for symptom resolution. If symptoms resolve within 6 hours, they may be discharged; if not, they should be admitted and observed. Patients suffering from severe anticholinergic poisoning and those treated with physostigmine should be admitted to the intensive care unit for closer observation.
References
1. Mowry JB, Spyker DA, Brooks DE, Zimmerman A, Schauben JL. 2015 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 33rd Annual Report. Clin Toxicol (Phila). 2016 Dec;54(10):924-1109. doi: 10.1080/15563650.2016.1245421.
2. Ghossein N, Kang M, Lakhkar AD. Anticholinergic Medications. [Updated 2021 May 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan.
3. Shervette RE 3rd, Schydlower M, Lampe RM, Fearnow RG. Jimson “loco” weed abuse in adolescents. Pediatrics 1979; 63:520.
4. Gerretsen P, Pollock BG. Drugs with anticholinergic properties: a current perspective on use and safety. Expert Opin Drug Saf. 2011 Sep;10(5):751-65.
5. Schweitzer P, Mark H. The effect of atropine on cardiac arrhythmias and conduction. Part 1. Am Heart J. 1980 Jul;100(1):119-27.
6. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, Van Kerrebroeck P, Victor A, Wein A., Standardisation Sub-Committee of the International Continence Society. The standardisation of terminology in lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Urology. 2003 Jan;61(1):37-49.
7. Campbell NL, Boustani MA, Lane KA, Gao S, Hendrie H, Khan BA, Murrell JR, Unverzagt FW, Hake A, Smith-Gamble V, Hall K. Use of anticholinergics and the risk of cognitive impairment in an African American population. Neurology. 2010 Jul 13;75(2):152-9.
8. Broderick ED, Metheny H, Crosby B. StatPearls [Internet]. StatPearls Publishing; Treasure Island (FL): Nov 23, 2020. Anticholinergic Toxicity.
9. Leybishkis B, Fasseas P, Ryan KF. Doxylamine overdose as a potential cause of rhabdomyolysis. Am J Med Sci 2001; 322:48.
10. Bernhardt DT. Topical diphenhydramine toxicity. Wis Med J. 1991 Aug;90(8):469-71.
11. Sharma AN, Hexdall AH, Chang EK, Nelson LS, Hoffman RS. Diphenhydramine-induced wide complex dysrhythmia responds to treatment with sodium bicarbonate. Am J Emerg Med. 2003 May;21(3):212-5. doi: 10.1016/s0735-6757(02)42248-6.
12. Beaver KM, Gavin TJ. Treatment of acute anticholinergic poisoning with physostigmine. Am J Emerg Med. 1998 Sep;16(5):505-7. doi: 10.1016/s0735-6757(98)90003-1.
13. Burns MJ, Linden CH, Graudins A, Brown RM, Fletcher KE. A comparison of physostigmine and benzodiazepines for the treatment of anticholinergic poisoning. Ann Emerg Med. 2000 Apr;35(4):374-81. doi: 10.1016/S0196-0644(00)70057-6.
14. Arens AM, Shah K, Al-Abri S, Olson KR, Kearney T. Safety and effectiveness of physostigmine: a 10-year retrospective review. Clin Toxicol (Phila). 2018 Feb;56(2):101-107. doi: 10.1080/15563650.2017.1342828. Epub 2017 Jul 13.