Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewer: Mary Claire O’Brien, MD
Introduction
Kidney stones are common causes of abdominal pain, with total prevalence in the US 5%, making it quite a routine ED diagnosis. Common in patients 20-50, rare >60 years old. Often, patients present with flank pain and some urinary symptoms. They are significant source of morbidity and impair quality of life for many patients. We discuss the risk factors, presentation, and management of these patients.
Pathophysiology
80% of stones are calcium, with oxalate > phosphate. Other lesser types in no particular order include uric acid, struvite (magnesium ammonium phosphate), and cysteine. Of course, patients can have stones composed of a mixture of these.
For boards and shelf, you do not need to know the details beyond these types of stones other than that they exist. You will not be tested on pictures of stone shapes under microscopy, or common associations of stones with systemic disease.
There are several theories on stone formation, none are testable. In general, much like gallstones, there is soluble material (calcium oxalate) that supersaturates in urine and forms crystals.
Risk factors
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Anything that increases supersaturation. High urinary calcium or low calcium dietary intake, higher oxalate intake or high urine oxalate, lower urinary citrate, high animal protein intake, and low potassium intake.
Prior nephrolithiasis: 15% recurrence at one year, 50% recurrence at 10 years.
Family history: >2x increased risk of stones.
Any bariatric surgery (e.g. bypass), short bowel syndrome: higher risk of oxalate GI absorption and therefore more stones.
Certain medications: indinavir, acyclovir, sulfadiazine, triamterene.
Any metabolic diseases: gout, obesity, DM, HTN.
Presentation
Symptoms typically develop when the stone moves from the renal pelvis into the ureter. Importantly, stones in the kidneys do not cause symptoms.
Classically colicky pain (waxes and wanes) found in the flank and radiating to the groin. Episodes of pain typically last several minutes to an hour and patients cannot lie still. Pain immediately resolves upon stone passage.
Exam is unreliable, only about 50% have CVA tenderness.
Hematuria (gross 30% of patients, or microscopic 85% of patients) together with flank pain is strongly suggestive of nephrolithiasis. It is specific but poorly sensitive. Hematuria is more present early on (95% on day 1, 65% on days 3-4).
Other symptoms in no particular order include nausea/vomiting (50%), dysuria, and urgency/decreased urination.
The more distal the stone, the more common the urinary symptoms.
Complications
Stones cause post-obstructive kidney damage, leading to evident hydronephrosis with resulting laboratory abnormalities. Untreated nephrolithiasis can lead to CKD/ESRD. Hydronephrosis indicates obstruction that is at risk for impairing renal blood flow.
Diagnosis
CT of the abdomen and pelvis is the best, preferred test for patients presenting for the first time with symptoms concerning for nephrolithiasis.
This test is done without contrast. It reliably detects hydronephrosis, hydroureter, and nephrolithiasis with detailed measurements and density. Sensitivity and specificity are 94% and 97%, respectively.
IV contrast does decrease sensitivity for small stones, however for detecting stones >3 mm, contrast CT is 95% sensitive- not bad.
Modern CT scans are so darn good now that they can detect signs of urinary tract obstruction. Ureteral dilatation found in 85 and 97% at 2 and 8 hours respectively, perinephric stranding in ~30% between 2-8 hours.
Ultrasound of kidneys and bladder
Preferred initial test in pregnant patients. A classic board question. However, the test is really not that solid for definitively diagnosing nephrolithiasis. Sensitivity and specificity are 70% and 75%, respectively. Yikes.
Stone detection is ~55% at best for both EM doctors and radiologists.
What about x-ray? Abdominal plain films do not show hydronephrosis and are overall less accurate for stone detection. It’s a mixed bag, ranging from a miserable 29-59% accuracy in stone detection. We do not shoot plain films for diagnosing nephrolithiasis.
Radiolucent stones are often missed, stones <5 mm are often missed.
There is a lot of talk out there regarding US first followed by CT without contrast. Boards want you to do CT without contrast. It’s the definitive test and shows other abdominal pathology. US is great for “recurrent” nephrolithiasis patients, but even then CT should be considered (see below for more on this debated topic).
Management
BMP should be ordered for evaluating electrolytes and creatinine. AKI is rare, only found in 1-2% of all stones.
Urine studies should be performed to evaluate for blood in the urine and presence of infection.
Pain control: unless contraindicated due to comorbidities or AKI, we prefer IV ketorolac as our initial pain medication, along with acetaminophen. It is thought that NSAIDs reduce ureteral smooth muscle tone. Whether or not this is true is debated, but who cares because that sounds great. It is true however that NSAIDs are as effective as opioids. Some patients will require opioids as well as nausea medications.
Forced IV hydration does not effectively reduce the amount of pain medication or increase stone passage, so don’t fluid overload patients.
Stone passage
Size is the biggest determinant: most all stones <4 mm pass spontaneously.
<2 mm size: average stone passage ~7 days. 3% need intervention.
4-6 mm size: average stone passage ~15 days. 50% need intervention.
>6 mm size: 99% will need intervention as these do not pass on their own.
Location is also important: proximal ureter (50% chance of passage) versus the ureterovesical junction (80% chance).
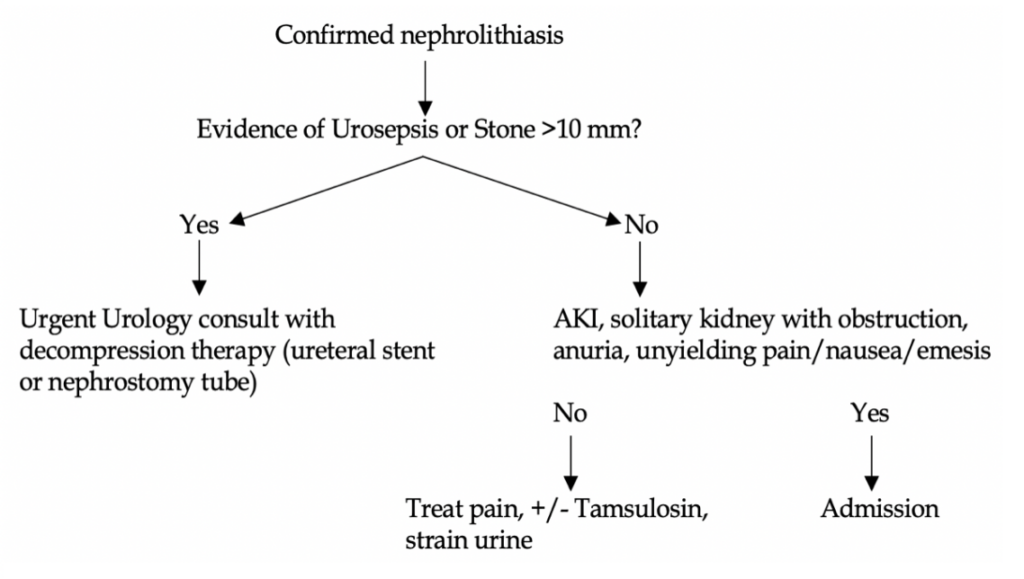
When to call urology in the ED? Also, who needs admission? The answers are the same for both (see algorithm).
Any stone with AKI, anuria, clinical evidence of urosepsis, unyielding pain or N/V after parenteral attempts, single kidney or transplant kidney with signs of obstruction.
The most concerning findings in a patient with a kidney stone is urosepsis. These patients need antibiotics, IV fluids, and urgent urology consult for decompression (ureteral stent, nephrostomy tube).
Who needs outpatient urology? Any patient with continued pain and confirmed stone should have outpatient urology follow up. Advise patients to strain their urine until follow up with urology or PCP.
Medication expulsion therapy
Tamsulosin (alpha blocker) has been used for years to facilitate stone passage with stones 5 – 10 mm in diameter. The drug has come under question whether or not it truly does help with passage, but right now urology still likes it and EM is pretty ambivalent/against it. It will not be on boards. We do not advise prescribing it unless urology asks for it prior to outpatient follow up (they likely will).
Bonus section!
What about patients coming to the ED with history of nephrolithiasis and recurrent symptoms that sounds like another episode? Do we need to CT-scan all these patients again every time? Its unclear. One study with 231 patients undergoing CT for “recurrent stone symptoms” 82% had no change in diagnosis, 12% had a non-urgent change in diagnosis, and 7% had a diagnosis that required urgent intervention. Appendicitis was the most common mimicker.
7% is an unacceptable number to not scan patients with “recurrent stone symptoms”. We simply cannot safely excuse patients’ symptoms for nephrolithiasis. Therefore, treat these patients’ workups as case-by-case. US can really help in these cases and decrease CT frequency.
Quick diagnostic summary
No history of kidney stones with a convincing story —> CT abdomen/pelvis without contrast
Concern for nephrolithiasis in a pregnant female —> Ultrasound of kidneys, bladder
Past history of prior nephrolithiasis and similar symptoms —> US first, +/- CT depending on presentation, labs, other risk factors
References
1. Koroglu M, Wendel J, Ernst R, Oto A. Alternative diagnoses to stone disease on unenhanced CT to investigate acute flank pain. Emergency radiology. 2004;10(6):327–333.
2. Baun K, Easter J. Marx: Rosen’s Emergency Medicine-Concepts And Clinical Practice. 8th ed. Elsevier Health Sciences; 2013:1336-1342.
3. Manthey DE, Nicks BA. Chapter 97. Urologic Stone Disease. In: Tintinalli JE, Stapczynski J, Ma O, Cline DM, Cydulka RK, Meckler GD, T. eds. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 7e. New York, NY: McGraw-Hill
4. Coll D, Varanelli M, Smith R. Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. American Journal of Roentgenology. 2002;178(1):101–103.
5. Kidney Stones: American Urological Association. 2014. Available at: http://www.auanet.org/education/kidney-stones.cfm. Accessed October 31, 2014.
6. Goldstone A, Bushnell A. Does diagnosis change as a result of repeat renal colic computed tomography scan in patients with a history of kidney stones? Am J Emer Med. 2010 Mar; 28 (3):291-5.
7. Tang X, Lieske J. Acute and chronic kidney injury in nephrolithiasis. Current Opinion in Nephrology and Hypertension. 2014;23(4):385-390. doi:10.1097/01.mnh.0000447017.28852.52.
8. Singh P, Enders FT, Vaughan LE, et al. Stone Composition Among First-Time Symptomatic Kidney Stone Formers in the Community. Mayo Clin Proc 2015; 90:1356.
9. Lieske JC, Rule AD, Krambeck AE, et al. Stone composition as a function of age and sex. Clin J Am Soc Nephrol 2014; 9:2141.
10. Teichman JM. Clinical practice. Acute renal colic from ureteral calculus. N Engl J Med 2004; 350:684.
11. Uribarri J, Oh MS, Carroll HJ. The first kidney stone. Ann Intern Med 1989; 111:1006.
12. Asplin JR, Coe FL. Hyperoxaluria in kidney stone formers treated with modern bariatric surgery. J Urol 2007; 177:565.
13. Kopp JB, Miller KD, Mican JA, et al. Crystalluria and urinary tract abnormalities associated with indinavir. Ann Intern Med 1997; 127:119.
14. Fulgham PF, Assimos DG, Pearle MS, Preminger GM. Clinical effectiveness protocols for imaging in the management of ureteral calculous disease: AUA technology assessment. J Urol 2013; 189:1203.
15. Wong C, Teitge B, Ross M, et al. The Accuracy and Prognostic Value of Point-of-care Ultrasound for Nephrolithiasis in the Emergency Department: A Systematic Review and Meta-analysis. Acad Emerg Med 2018; 25:684.