Want to experience the greatest in board studying? Check out our interactive question bank podcast- the FIRST of its kind here: emrapidbombs.supercast.com
Author: Blake Briggs, MD
Peer Reviewers: Travis Smith, DO; Mary Claire O’Brien, MD
Objectives: define non-sustained versus sustained VT, understand how to identify VT on EKG, describe pathologic causes of VT, follow algorithmic approach to treating VT, understand principles of polymorphic VT.
Introduction
Ventricular tachycardia (VT) is a fast, regular, abnormal heart rate. It arises due to improper electrical conduction in the ventricles. There are 2 categories of VT depending on how long it lasts, and 3 overall types, or flavors, of VT:
1. Monomorphic 2. Torsades polymorphic 3. Generic polymorphic
Non-sustained: wide QRS >120 ms, >100 bpm, <30 seconds. Potential marker for sustained VT, but not a predictor of sudden cardiac arrest (SCA). No evidence supports acute intervention. If structural heart disease is present or if left ventricular ejection fraction <40%, however, it can be more of a risk and if recurrent warrants a discussion with cardiology.
Sustained: wide QRS >120 ms, >100 bpm, >30 seconds. Can be monomorphic or polymorphic:
Monomorphic- consistent QRS amplitude and morphology. >90% of all ventricular arrhythmias.
Accelerate your learning with our EM Question Bank Podcast
- Rapid learning
- Interactive questions and answers
- new episodes every week
- Become a valuable supporter
Polymorphic- continuously variable QRS morphology and amplitude. <10% of all ventricular arrhythmias.
How to identify VT from SVT w/aberrancy: It is good to know that there are many features on EKG that suggest VT, see below:
-broad QRS complexes >160 ms
-capture beats: SA node transiently captures the ventricle, producing a normal QRS complex.
-fusion beats: sinus and ventricular rhythm combine to make a weird variant.
-AV dissociation with p waves marching through
-Josephson’s sign: notching of the nadir of S wave
-Brugada’s sign: distance from onset of QRS to S wave nadir is >100 ms.
-RSR’ complex with L>R taller R wave.
-Each QRS is nearly identical.
Despite all these criteria and the various published algorithms (Brugada, Wellens, etc), all are ~90% specific for VT (not the best). A much more reliable method is that anyone with any ischemic heart disease history, heart failure, or just being elderly has about a 98% chance that the wide regular complex tachycardia you see is VT. Additionally, those <40 years old still have up to a 50% occurrence of VT on EKGs compared to SVT with aberrancy. So, bottom line, vast majority of wide complex tachycardia is VT. Treat for VT, sort it out later. VT is the rhythm that will kill your patient first, not SVT with aberrancy!
Presentation: often patients are asymptomatic or +/- palpitations. Chest pain, lightheadedness, blurry vision, dyspnea, nausea/vomiting can occur too. Stable vs unstable can be difficult to define. This is frightening because VT can rapidly progress to sudden cardia arrest without any warning.
In any situation, a 12-EKG should be performed. Telemetry is good but not definitive for identifying rhythm changes.
If sustained VT is determined, crash cart, airway supplies, and multiple large-bore IVs should be established.
Pads should immediately be placed on the patient.
Look for underlying causes: you need to start early when looking for causes. This is especially true when standard measures are not improving the patient’s condition. In particular, the great EKG mimicker hyperkalemia (classically “slow VT” with <140 bpm) and TCA or another Na-channel blocker overdose.
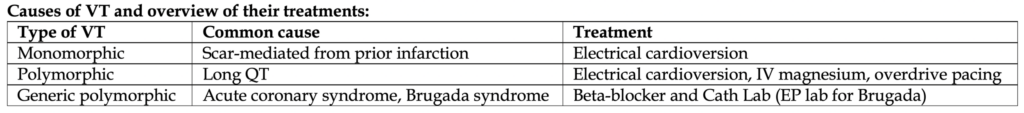
Monomorphic VT: the most common form of VT. Classically caused by a fibrotic scar from prior infarction and cardiac ischemia. Usually not due to acute coronary syndrome.
For the boards, they will want the traditional approach of antiarrhythmic first, followed by cardioversion if they are unsuccessful or the patient’s clinical status worsens at any point.
More details on antiarrhythmic agents: Amiodarone: slow onset of action but it reduces the rate of recurrence of VT. When to use:
-Polymorphic VT (see algorithm below)
-Implantable cardiac defibrillator (ICD) patient with VT above detection rate
-VT in cardiac arrest (ACLS protocol)
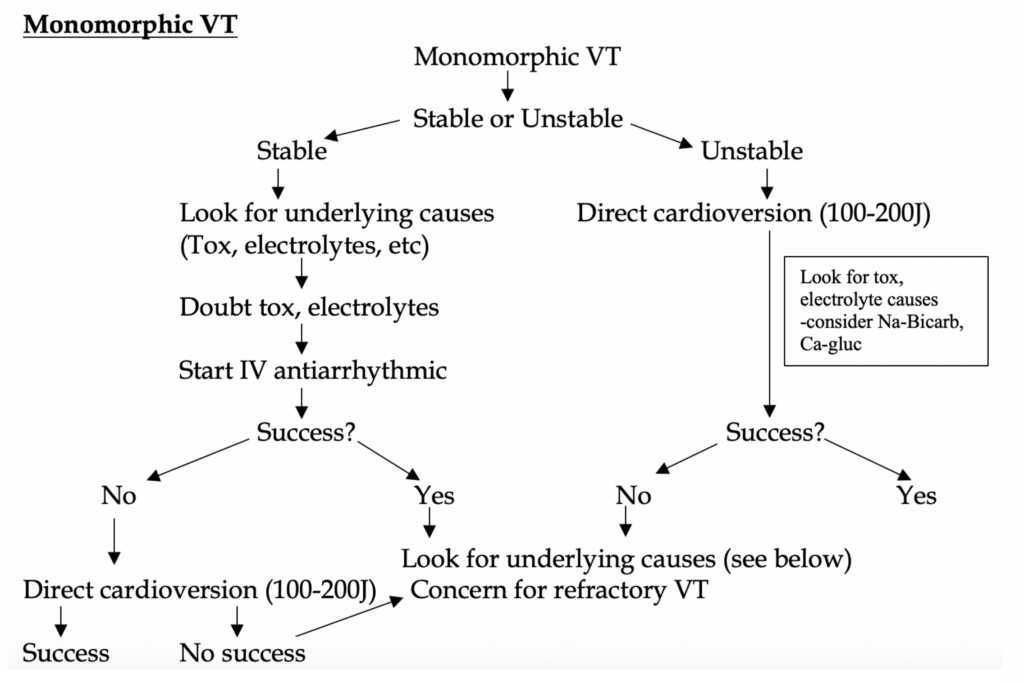
Procainamide: faster rate of VT termination, lower rates of major adverse events, lower rates of serious adverse cardiac events.
When to use: Scar-mediated VT: >50 years old with cardiac history. We’ll spare you the details, but a great study in 2016 (PROCAMIO) found procainamide superior to amiodarone in stable, monomorphic VT. In general, procainamide should be first line chemical therapy in patients with stable ventricular tachycardia. Downside: Not all hospital formularies carry it
Lidocaine: evidence has been lacking, but a new study shows some small evidence for lidocaine being equal to amiodarone in monomorphic VT. Lidocaine does not cause hypotension as much as amiodarone or procainamide, and it has a shorter administration time.
For patients in whom VT terminates during the drug infusion, the drug can be stopped or continued if the patient has been having recurrent episodes. Side Effects: All anti-arrhythmic agents have various side effects; hypotension is the most common.
Polymorphic VT: divided into torsades (prolonged QT) and generic (normal QT).
Torsades: remember the causes of prolonged QT like medication: sotalol, risperidone, macrolides, chloroquine, protease inhibitors, antiarrhythmics (any Class I or III), thiazides. Other causes include hypokalemia, hypocalcemia, hypomagnesemia.
Treatment: appropriately cardiovert if unstable at any point. Magnesium IV push followed by a drip. Replace electrolytes as indicated. Do not give beta-blockers or antiarrhythmics here, they won’t help with the QT and might worsen it (remember beta-blockers lower the heart rate which means the QT will get longer). For intermittent, persistent torsades, overdrive pacing is an option (maintaining HR above a certain level to shorten the QT).
Generic: most commonly due to acute coronary syndrome. Brugada syndrome is rare cause.
Treatment: Appropriately cardiovert if unstable at any point. Beta-blockers are a good idea here since we are must likely dealing with ACS. Repeat EKG if patient exits VT and look for ST elevation.
Special VT scenarios: The 2 Flavors of VT in ICD patients:
-VT that is below ICD detection rate (usually <170’s). Treat this like any VT
-VT that is above ICD detection rate (>170’s). A little trickier because it could be the ICD isn’t working properly, there is baseline severe heart disease, or underlying electrolyte abnormalities. Address the underlying issue as indicated.
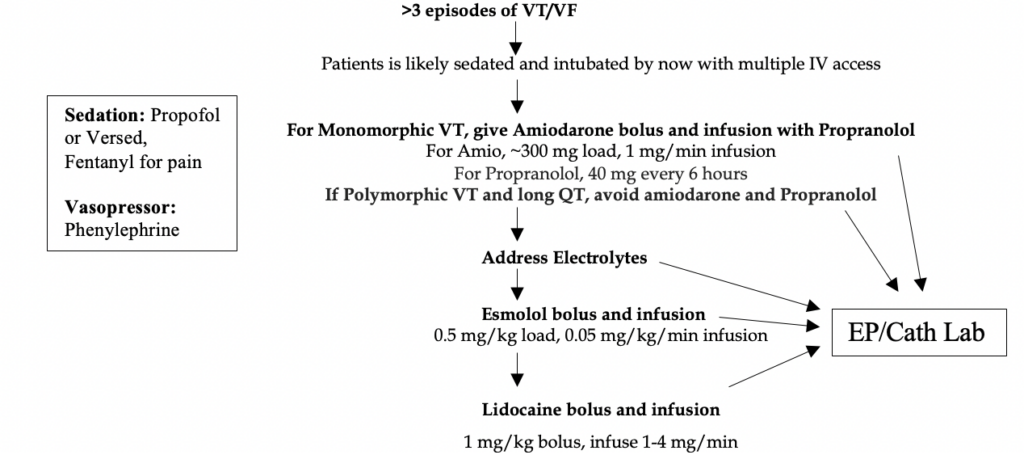
Electrical storm: >3 distinct episodes of sustained VT, VF, or receive appropriate shocks from an ICD within 24 hours. These patients are often chronically very ill- cardiomyopathy, low EF, prior MIs with heavy CAD burden, and patients with ICDs. Triggers include the usual stressors seen elsewhere in medicine (electrolyte abnormalities, binge drinking, infections, ischemia, drug toxicities, even certain antiarrhythmic medications.
The key component of pathology is very elevated sympathetic tone, with a vicious cycle of tachycardia, emotional distress and pain from cardioversion releasing more catecholamines.
Really the treatment is the same as above, with more emphasis on following ACLS protocol and strong consideration for EP lab. See algorithm below…